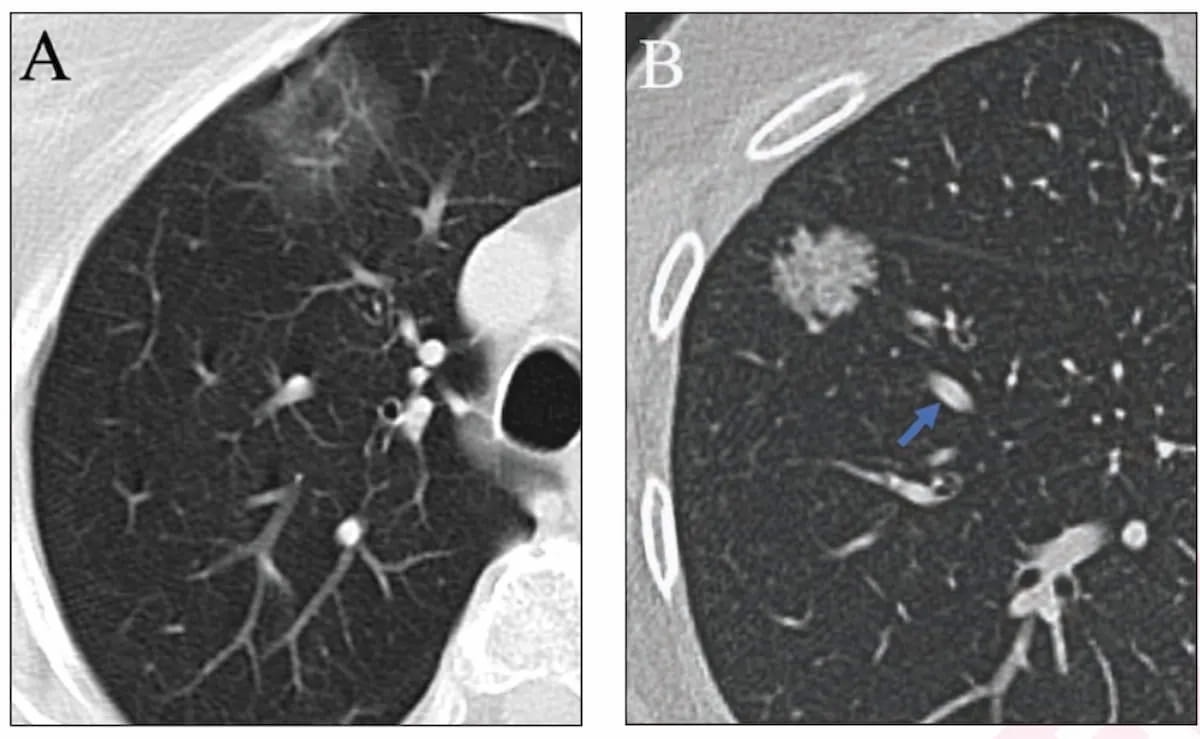
While overlapping features with ground glass nodules (GGNs) on lung computed tomography (CT) can make it challenging for risk stratification of lung adenocarcinomas, an emerging deep learning (DL) model with simulated adjudication for addressing discordant nodule classifications may provide a viable alternative.
For the retrospective study, recently published in Radiology, researchers compared six CT-based models for predicting invasive progression of lung adenocarcinoma: a radiomics model (model 1); a deep learning model (model 2); a combined model of radiomics and deep learning (model 3); model 1 plus two binary models and a ternary classification model for simulating reader classification and adjudication (model 4); model 2 plus the aforementioned binary and ternary model additions (model 5); and model 3 plus the aforementioned binary and ternary model additions (model 6).
The models were developed from a multicenter training set of 3,384 lung nodules with subsequent internal testing with 966 lung nodules and validation with a set of 579 lung nodules, according to the study. The researchers compared the models in an external test set of 361 pure ground glass nodules (pGGNs) from 281 patients (mean age of 55.2).
The researchers found that model 6 offered the highest accuracy, sensitivity, and specificity for minimally invasive adenocarcinoma (MIA). In comparison to the combination of radiomics and deep learning in model 3, the addition of binary models and the ternary adjudication model to model 6 to address discordant classifications lead to six, 12 and 4 percent increases in accuracy (85 percent vs. 79 percent), sensitivity (75 percent vs. 63 percent) and specificity (89 percent vs. 85 percent), respectively, for MIA classifications.
Model 6 also demonstrated 86 percent accuracy, 78 percent sensitivity and 90 percent specificity for detecting preinvasive adenocarcinomas, according to the researchers.
“The more accurate prediction of minimally invasive nodules not only improved overall model performance but can also be important in clinical practice in guiding timing of surgery, resection methods allowing preservation of lung function, and improving quality of life.,” wrote study co-author Zhengyu Jin, M.D., who is affiliated with the Department of Radiology at the Peking Union Medical College Hospital in Beijing, China, and colleagues.
The researchers said the addition of the binary models for classification and the ternary adjudication model for discrepancy resolution to a combined radiomics and deep learning model is akin to the random forest method’s use of multiple decision trees.
Three Key Takeaways
- Improved risk stratification with deep learning. The integration of deep learning (DL) models, particularly when combined with simulated adjudication for addressing discordant nodule classifications, can significantly improve risk stratification of lung adenocarcinomas. Model 6, which incorporated both DL and simulated adjudication, demonstrated the highest accuracy, sensitivity, and specificity for predicting minimally invasive adenocarcinoma (MIA).
- Enhanced clinical decision-making. Accurate prediction of minimally invasive nodules, as facilitated by DL models, holds clinical significance by guiding the timing of surgery, optimizing resection methods to preserve lung function, and ultimately improving patients' quality of life. The higher accuracy in identifying MIA nodules can aid clinicians in making informed decisions regarding patient management.
- Methodological advancement. The approach of combining radiomics and deep learning models, augmented with binary classification models and a ternary adjudication model, represents a methodological advancement akin to the random forest method's utilization of multiple decision trees, according to the study authors. This strategy harnesses the strengths of each submodel while enhancing the overall model's transparency and interpretability, thereby potentially improving its applicability in clinical practice.
“Our DL models have the potential to assist in the management of pulmonary nodules. … Due to the different preferences of invasiveness discrimination of each submodel, this strategy can better leverage the advantages of each submodel compared with a separate ternary classification model while improving the transparency and interpretability of the overall model,” noted Jin and colleagues.
The study authors also pointed to the significantly lower range of sensitivity (7.3) and specificity (0.9) in the ternary classification for model 6, noting that it had “the most balanced performance of all six models.”
(Editor’s note: For related content, see “What Emerging CT Research Reveals About Pure Ground Glass Nodules,” “Researchers Cite 81 Percent Survival Rate Years After Initial Lung Cancer Diagnosis with Low-Dose CT” and “AI-Based Denoising Technique Achieves 76 Percent Reduction in Radiation Dosing for CT Lung Cancer Screening.”)
In regard to study limitations, the authors acknowledged no direct comparison of the deep learning model to radiologist performance and no assessment of smoking impact upon the deep learning model. Noting that the deep learning models were primarily assessed on pGGN in Asian individuals, the researchers acknowledged that extrapolation of the findings to broader populations may be limited. The study authors also noted a possible “clustering effect” with the data given the inclusion of patients with more than one nodule.