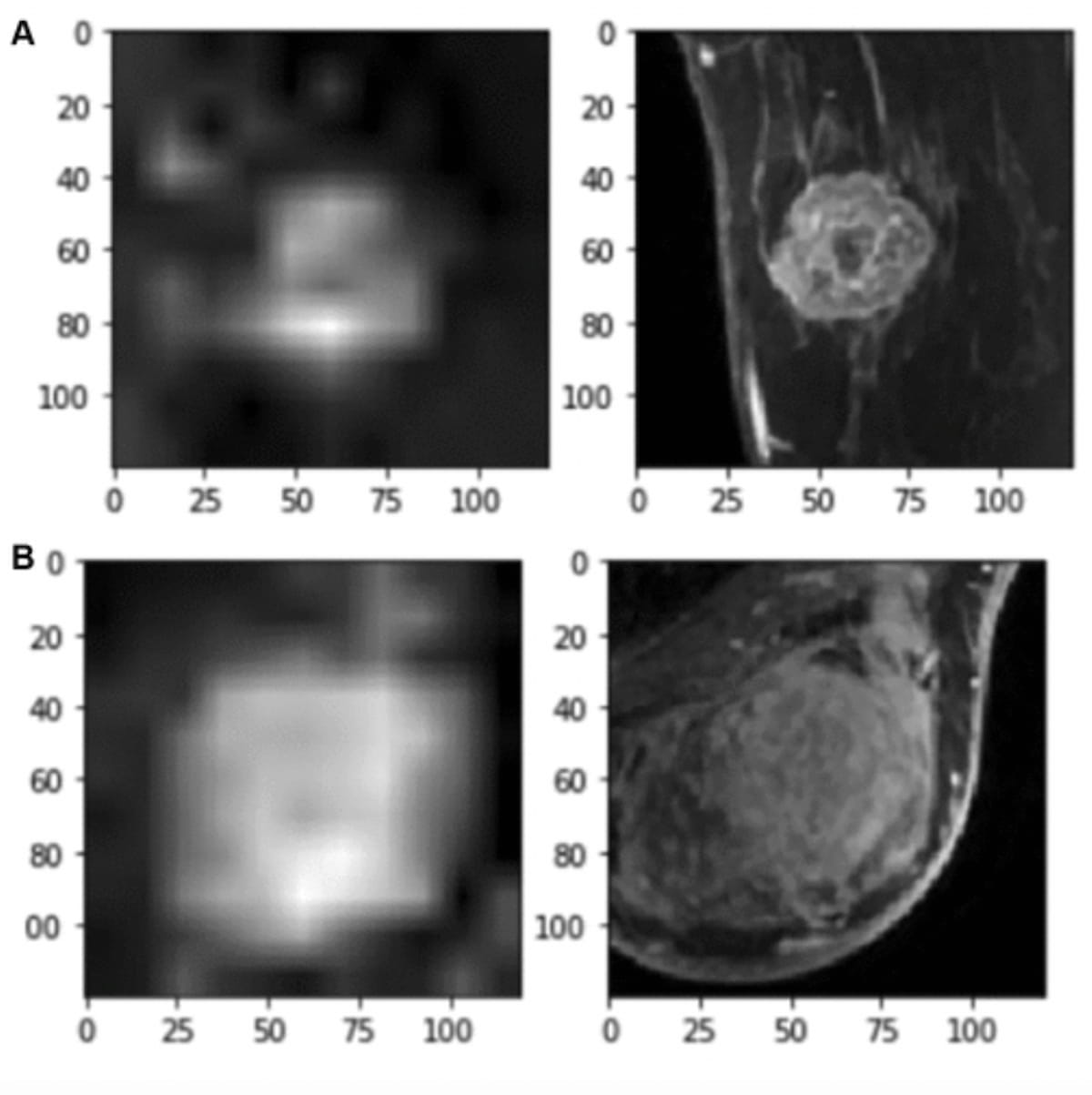
In contrast to a machine learning model based on clinicopathologic features alone, a four-dimensional (4D) convolutional neural network (CNN) model that integrates clinical and breast magnetic resonance imaging (MRI) findings achieved a 24 percent higher area under the curve (AUC) in predicting axillary node status in women with breast cancer.
For the retrospective study, recently published in Radiology: Imaging Cancer, researchers evaluated the 4D CNN model for 350 women (mean age of 51.7) who had dynamic contrast-enhanced MRI (DCE-MRI) exams between July 2013 and July 2016.
The study authors found that the 4D CNN model had an 87 percent AUC, an 89 percent sensitivity rate and a 76 percent specificity rate for differentiating between pNO and pN+ status. In comparison, a machine learning model built on clinicopathologic factors alone had a 63 percent AUC, a 75 percent sensitivity rate and a 52 percent specificity rate.
The 4D hybrid model that incorporated breast MRI findings also had a significantly lower false-negative rate (11 percent) in contrast to the clinical model (25 percent), according to the researchers.
“ … A robust imaging-based predictive model that assesses the presence of lymph node metastasis with high sensitivity would help select patients who could potentially avoid (sentinel lymph node biopsy) SLNB and facilitate treatment decisions for patients with breast cancer, without the need for an invasive procedure,” wrote study co-author Basak Dogan, M.D., FSBI, the director of breast imaging research, an associate professor of radiology and the Eugene P. Frenkel Endowed Scholar in Clinical Medicine at the University of Texas Southwestern Medical Center, and colleagues.
The researchers also examined the effectiveness of the 4D CNN model at different cutoff points for specificity. At 51 percent specificity, the 4D hybrid model had a 95 percent sensitivity rate and a 5 percent false-negative rate, according to the study authors. They noted a 91 percent sensitivity rate and a 9 percent false-negative rate when employing a 71 percent cutoff rate for specificity.
“(These findings) align with the 90% sensitivity and less than 10% false-negative rate benchmarks used to define success for most SLNB studies, while maintaining higher diagnostic performances than axillary (ultrasound), morphologic evaluation of DCE MRI, or other prognostics nomograms,” pointed out Dogan and colleagues.
Three Key Takeaways
- Improved predictive power. Integrating clinical and breast MRI findings into a 4D CNN model significantly enhances its predictive capability for axillary node status in breast cancer patients, as evidenced by a 24 percent higher AUC compared to models based solely on clinicopathologic features.
- Reduced false-negative rate. The 4D hybrid model demonstrates a notably lower false-negative rate (11 percent) compared to the clinical model (25 percent), indicating its potential to more accurately identify patients with axillary lymph node metastasis, thereby reducing the likelihood of unnecessary sentinel lymph node biopsies.
- Triage tool for earlier diagnosis. With its high sensitivity and lower false-negative rate, the 4D hybrid model could serve as a valuable triage tool, enabling earlier diagnosis of axillary metastases and potentially reducing benign sentinel lymph node biopsy procedures by over 50 percent. This benefit is particularly significant considering the potential complications associated with unnecessary invasive procedures such as lymphedema, seroma, infection, and pain.
The 4D hybrid model also demonstrated significantly better differentiation of clinically node positive and negative status in comparison to the clinical model. While the 4D hybrid model had lower specificity (62 percent vs. 77 percent), the study authors noted a 24 percent higher AUC (79 percent vs. 55 percent), a 45 percent higher sensitivity rate (80 percent vs. 35 percent) and a 45 percent lower false-negative rate (20 percent vs. 65 percent).
The study authors maintained that the 4D hybrid model could be a significant triage tool in facilitating earlier diagnosis of axillary metastases and reducing benign SNLB procedures by more than 50 percent.
“This is an important benefit as some patients undergoing SLNB develop permanent complications, including lymphedema, seroma, wound infection, and pain, despite having a low probability of a positive result, which may substantially impact their management,” emphasized Dogan and colleagues.
(Editor’s note: For related content, see “Ultrasound Nomogram May Enhance Prediction of Metastatic Axillary Lymph Nodes in Breast Cancer Patients,” “Current Perspectives on PET/CT Imaging in Patients with Metastatic Breast Cancer” and “Is PET/CT Better than CT for Monitoring Metastatic Breast Cancer Treatment?”)
In regard to study limitations, the researchers said the machine learning model was tested on two affiliated hospitals with similar results and emphasized the need for further external validation of the model. The current model’s emphasis on a manual bounding box around the tumor is a key limitation that limits clinical adoption, according to the study authors. Noting that their datasets were comprised of imaging from 1.5 T MRI devices, the researchers acknowledged that their results may have limited applicability to imaging obtained with 3 T MRI devices.