- AI
- Molecular Imaging
- CT
- X-Ray
- Ultrasound
- MRI
- Facility Management
- Mammography
Can AI Improve Detection of Extraprostatic Extension on MRI?
Utilizing a deep learning-based AI algorithm to differentiate between diagnostic and non-diagnostic quality of prostate MRI facilitated a 10 percent higher specificity rate for diagnosing extraprostatic extension on multiparametric MRI, according to research presented at the recent RSNA conference.
Differentiating between diagnostic and non-diagnostic prostate magnetic resonance imaging (MRI) with artificial intelligence (AI) may significantly improve the detection of extraprostatic extension (EPE),
In a retrospective study, recently presented at the Radiological Society of North America (RSNA) conference, researchers reviewed data from 812 patients (median age of 62) who had multiparametric MRI (mpMRI) and a subsequent radical prostatectomy. Using a validated grading system for EPE on MRI, the study authors considered an EPE grade of 1 or above to be positive for EPE.
The researchers found that only 41 percent of positive EPE diagnoses on mpMRI led to confirmed EPE, according to the study.
When utilizing an AI algorithm to help discern image quality for T2 weighted imaging (T2WI) and apparent diffusion coefficient (ADC) maps, the researchers determined that 35 percent of the T2WI sequences (284 out of 812) and 32 percent of the ADC maps (260 out of 812) were non-diagnostic.
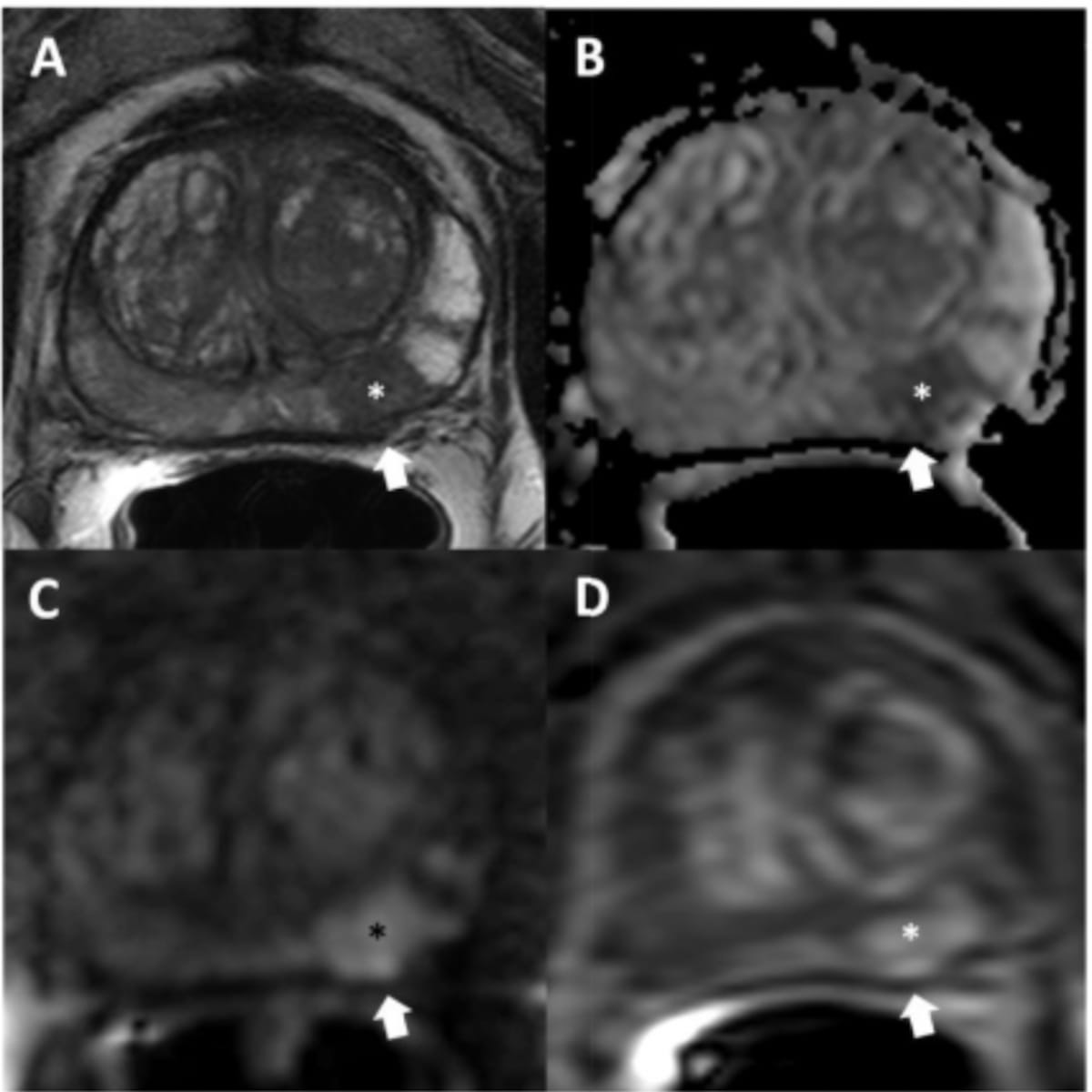
MRI imaging reveals a PI-RADS category 5 lesion with a slight capsular bulge (NCI EPE grade 1) in the left mid-base peripheral zone. While this case was a true positive diagnosis of extraprostatic extension (EPE), the authors of a recent study found that only 41 percent of positive EPE diagnoses on mpMRI led to confirmed EPE. (Images courtesy of RSNA.)
After comparing non-diagnostic and diagnostic T2WI scans, the researchers found that diagnostic quality T2WI scans had a 10 percent higher specificity rate (73 percent vs. 63 percent) and a seven percent lower false positive rate (21 percent vs. 28 percent) for EPE.
“Our study successfully employed a deep learning-based AI algorithm to classify image quality of prostate MRI and demonstrated that preoperative T2WI quality is crucial for accurate EPE evaluation,” wrote lead study author Yue Lin, BA, a MRSP scholar at the National Institutes of Health (NIH), and colleagues.
The study authors noted that utilizing AI to ascertain T2WI MRI quality may facilitate enhanced decision-making for patients with prostate cancer.
“Image quality assessment AI could be integrated into radiologist clinical workflow to improve prostate cancer imaging,” suggested Lin and colleagues.
Emerging Perspectives on PSMA PET Radiotracers: An Interview with Kenneth J. Pienta, MD
April 24th 2024In a recent interview, Kenneth J. Pienta, M.D., discussed the impact of piflufolastat F18, current directions in research with other PSMA-targeted radiotracers and future possibilities for the role of PSMA PET in the imaging paradigm for prostate cancer.
The Reading Room: Artificial Intelligence: What RSNA 2020 Offered, and What 2021 Could Bring
December 5th 2020Nina Kottler, M.D., chief medical officer of AI at Radiology Partners, discusses, during RSNA 2020, what new developments the annual meeting provided about these technologies, sessions to access, and what to expect in the coming year.
Study of Ofatumumab for Multiple Sclerosis Shows 'Profoundly Suppressed MRI Lesion Activity'
April 17th 2024The use of continuous ofatumumab in patients within three years of a relapsing multiple sclerosis diagnosis led to substantial reductions in associated lesions on brain MRI scans, according to research recently presented at the American Academy of Neurology (AAN) conference.
RSNA 2020: Addressing Healthcare Disparities and Access to Care
December 4th 2020Rich Heller, M.D., with Radiology Partners, and Lucy Spalluto, M.D., with Vanderbilt University School of Medicine, discuss the highlights of their RSNA 2020 session on health disparities, focusing on the underlying factors and challenges radiologists face to providing greater access to care.
Are Prostate Biopsies Necessary in Patients with Negative or Equivocal MRIs and Low PSA Density?
April 2nd 2024Up to 48 percent of unnecessary prostate biopsies could be eliminated by limiting biopsy to patients with PI-RADS 4 and higher MRI assessments and a prostate-specific antigen density level below 0.15 ng/mL2, according to a new meta-analysis.
