Artificial Intelligence & Mammography: Where It’s Been & Where It’s Going
From detecting breast density and reducing image file sizes to improving cancer detection and creating new risk models, AI is significantly impacting breast imaging.
As in all areas of health care, the primary goals of any clinician in diagnostic imaging are to provide quality patient care while also improving workflow and efficiency. This is also true for breast cancer screening and a key driver behind artificial intelligence’s (AI) role in the development of breast cancer screening technology.
It is also why AI will continue to impact technological innovations for years to come.
Consider, first, some of the current challenges imagers face with breast screening that the integration of AI has already been able to help overcome.
Typically, patients begin their breast cancer screening journey with a mammogram that not only indicates whether a woman may have breast cancer, but also identifies her level of breast density. This is an important piece of information to consider when developing a patient’s care pathway since having dense breasts is considered a risk factor, similar to having a family history of breast cancer.
Prior to the integration of AI, however, breast density categorization and identification has always been subjective. Clinicians needed to visually assess all images to be able to determine into which of the four categories the breast tissue should be categorized according to the Breast Imaging Reporting and Data System (BI-RADS) score: almost entirely fatty, areas of scattered fibroglandular density, heterogeneously dense, and extremely dense. This process is a subjective classification – depending on the individual reviewing the images – that could, in turn, impact the course of screening and supplemental studies for patients.
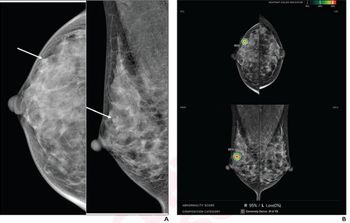
Additionally, when interpreting images for breast cancer lesions, more challenges could arise, many of which still exist today. For example, using digital breast tomosynthesis (DBT) – though more effective than 2D mammography at detecting invasive breast cancers – yields an overwhelming number of data files and large file sizes. This information is necessary to provide a clearer and more comprehensive assessment of the breasts, and it is also essential for radiologists to be able to quickly and efficiently pinpoint suspicious areas in a sea of breast tissue captured by the images. The need for this rapid assessment of concerning areas is so that they can be prioritized to quickly determine if additional imaging and biopsies are needed.
The introduction of AI technology into mammography has helped mitigate both challenges – subjective breast tissue density assessment and the burden of large numbers of images – for breast imagers. For example, AI-based technology, such as the Quantra™ 2.2 breast density assessment software, can use an algorithm powered by machine learning to standardize breast tissue density scores for patients. This capability can help provide more consistent and reliable scoring, which can ultimately help to determine the appropriate personalized screening pathway for each patient.
Likewise, AI can also help cut down on the overwhelming amount of images breast imagers review. For example, using Genius AI™-powered software, 3DQuorum™ Imaging Technology identifies clinically relevant regions of interest and preserves important features. By creating 6mm SmartSlices from original high-resolution 3D™ 1mm images – and retaining critical image detail – the system reduces the image volume for review by two-thirds1,2, saving imagers one hour of interpretation time daily.2,3,4
These examples demonstrate how AI is addressing challenging changes with workflow without compromising the great strides that have been made with accuracy. Looking to the future, there are a variety of other challenges that AI has the potential to similarly overcome.
As technology advances and vast databases of breast images and tissue patterns are available, algorithms will grow stronger in their ability to spotlight highly suspicious areas and cases for deeper examination. This will allow radiologists to focus on the suspicious areas and move past the rest, leading to even more accurate interpretations, greater cancer detections, and fewer false positives.
Furthermore, by collecting and streamlining large amounts of data for patients individually, including all of their various risk factors and background information, AI may have the capability to create new risk models that will allow patients to have a more personalized screening plan, including screening modality, screening frequency, and beyond.
Additionally, current risk models use simple metrics, such as a woman’s breast density. But, machine and deep learning offer the opportunity for improved risk prediction, for example, by finding patterns in mammograms that are predictive of breast cancer but are not identified by radiologists today.
These future capabilities of AI are promising and have the potential to truly impact patient care – from a more efficient workflow to more accurate results and personalized care. As these priorities will always be top goals for facilities and clinicians, future AI solutions – in addition to the current benefits it has already brought to the industry – should be met with excitement and enthusiasm by healthcare providers and administrators.
1. Tech File: TFL-00059
2. Physician Labeling: MAN-06153
3. Report: CSR-00116
4. FDA approval number.P080003/S008
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.














