Cardiac CT's promise awaits aid of outcomes studies
Advances in spatial, temporal resolution should help CT provide better functional, anatomic information
Cardiac CT's promise awaits aid of outcomes studiesBy: Franz von Ziegler, M.D.
Advances in spatial, temporal resolution should help CT provide better functional, anatomic information
Multislice CT scanners used in cardiac imaging are 16- to 64-slice systems that provide for a slice collimation of 0.5 to 0.75 mm (high spatial resolution) and rotation times of 330 to 420 msec (high temporal resolution). Therefore, a high-resolution data set of the beating heart can be achieved in a single breath-hold period.
The use of retrospective ECG triggering makes possible depiction of the heart in every cardiac phase and cross-sectional image reconstruction, leading to motion-free 2D and 3D images, usually in diastole, or at 65% of the cardiac cycle. ECG-correlated images require a regular heart rate, however, and most experienced centers recommend the use of beta blockers to lower the heart rate below a threshold of 60 to 65 bpm. This step provides for more stable and predictable image quality and also serves to lower radiation exposure. The introduction of technology such as dual-source CT (DSCT) scanners, which work with two radiation tubes and therefore improve temporal resolution to 83 msec, might overcome these limitations.
MORPHOLOGY AND FUNCTION
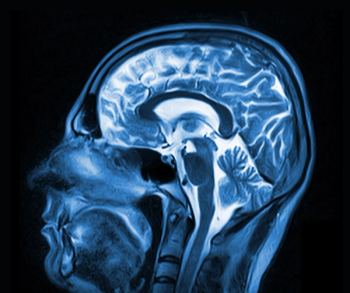
CT permits exact morphologic imaging of the heart and can document intracardiac calcification well. After injection of contrast agents, anatomic relationships and the dimension and configuration of cardiac chambers can be clearly assessed. Reconstruction of systolic and diastolic images permits assessment of global and regional ventricular function (see figure).1,2
With the exception of cardiac calcification, however, CT plays a very limited clinical role with respect to cardiac function and morphology, as echocardiography in most cases provides all clinically relevant information. If further need for clarification arises, MRI is the next step. But CT can be an alternative in cases in which ECG provides unsatisfactory results and MRI is impossible to perform because of metallic implants or claustrophobia, to provide detailed information on cardiac morphology and function.
HEAD-TO-HEAD
The assessment of coronary calcification, which correlates well with atherosclerotic plaque burden and its quantification by various methods (Agatston score, volume, or mass), is now widely accepted for the purpose of risk stratification because its predictive value is significantly higher than that of traditional risk factors.3-6 It remains unclear, however, which patients require such refined risk stratification and benefit from performing calcium scoring.
Most likely, calcium scoring will be useful in those patients who are considered to be at intermediate risk following traditional risk assessment. Neither calcium scoring in patients who are clearly at high risk nor unselected screening of the general population is reasonable. Also inappropriate is repeated or follow-up coronary calcium scanning. It is important to note that in asymptomatic individuals, the demonstration of even very large amounts of calcium is no reason by itself to perform invasive coronary angiography, because even pronounced coronary calcium, though a sign of high plaque burden, is not necessarily associated with the presence of significant coronary stenosis.
The beneficial utilization of high-resolution contrast-enhanced CT angiography of the entire coronary artery tree is attracting considerable interest. One of the central rationales for this application has been the noninvasive detection and grading of coronary artery stenosis. It must not be forgotten, however, that visualization of the small, tortuous, and rapidly moving coronary arteries stretches the temporal and spatial resolution of CT to its limits. Preselection by sinus rhythm, preparation of patients through heart rate control with beta blockers if needed and nitrates to dilate the coronary arteries, and very careful image acquisition are mandatory to achieve reliable results. The image quality of MSCT, for which a maximum spatial resolution of 0.4 x 0.4 x 0.4 mm is assumed under optimal conditions, does not equal that of conventional invasive coronary angiography.
In experienced hands, nevertheless, a high sensitivity (82% to 95%) and specificity (95% to 96%) for the detection of hemodynamically relevant coronary artery stenosis can be achieved. The percentage of unevaluable coronary artery segments is generally lower than 12%. Moreover, all studies, even with the use of 16-slice CT, consistently report a very high negative predictive value (96% to 99%).7,8 Although these results may be influenced by the relatively low prevalence of coronary stenoses in most studies, they nonetheless indicate that MSCT may be a reliable technology to noninvasively rule out the presence of significant coronary stenosis in such patient populations if performed with the latest generation of CT scanners.
Congenital coronary anomalies are infrequent but sometimes clinically significant. Assessment of atypical origin and course of anomalous coronary arteries can be difficult and time-consuming by invasive angiography, whereas several studies have shown that MSCT offers the possibility to reliably investigate the exact anatomic relationship.9,10
LIMITATIONS OF CTA
MSCT angiography, despite its encouraging results, has a number of limitations and cannot be expected to widely replace invasive cardiac catheterization in the near future. Pronounced coronary calcification and, especially in patients with high heart rates, motion artifacts can render images difficult or even impossible to interpret. Patients with atrial fibrillation or other arrhythmias cannot be evaluated. New and faster scanner generations such as DSCT may overcome these restrictions.
Coronary CTA is also a purely diagnostic tool. Unlike invasive catheter-based angiography, it offers no possibility for an immediate coronary intervention. Therefore, patients who, on the basis of their clinical presentation, have a very high likelihood of significant stenosis-those with absolutely typical chest pain and an unambiguously positive stress test-will not benefit from noninvasive angiography of any kind.
The high negative predictive value of coronary MSCT angiography, however, may make its clinical application in place of an invasive procedure quite useful in patients who are symptomatic but do not have a high pretest likelihood of coronary stenosis. If CTA can clearly rule out coronary heart disease, invasive angiography is not necessary. But unselected screening of asymptomatic individuals is not justified.
Unlike catheter angiography, CTA's cross-sectional nature enables assessment of the vessel wall as well. This offers a potential strength for noninvasive identification and characterization of atherosclerotic disease and is currently being evaluated. Several recent publications have shown that MSCT also permits visualization and characterization of fibrous, lipid-rich noncalcified plaque components by measuring CT attenuation within the lesion.11,12 But clinical applications are not supported by any prospective or outcome data. Performing contrast-enhanced CT studies in asymptomatic individuals with the purpose of plaque detection in a setting of risk stratification is therefore currently not justified. Before any clinical conclusion can be drawn from such observations, further corroboration is required.
BYPASSES AND STENT DEPICTION
Bypass vessels are somewhat larger than the native coronary arteries, and they move less rapidly. Thus, their visualization with CT is relatively straightforward. Occlusions and stenoses of bypass grafts can be detected with very high accuracy.13 Clinically, however, it is not be sufficient in most cases simply to assess the graft vessels themselves if a patient with previous bypass surgery presents with symptoms. It would also be necessary to depict the status of the native coronary arteries distal to the bypass anastomosis and of those branches that did not receive a graft. So far, it has not been shown conclusively that CT imaging permits assessment of the bypass grafts, the anastomotic site, and the native vessels. Coronary arteries in this special case may be challenging, because they tend to calcify heavily.
Visualization of intracoronary stents is theoretically possible, especially with later CT scanners, but image quality is often impaired by artifacts because of the stents' high-density metallic nature. Some initial studies in small patient populations have shown encouraging results, but even larger stents may be impossible to evaluate with regard to in-stent restenosis.14,15 More data are needed before any clinical recommendation can be made concerning the use of MSCT for follow-up after stent placement.
Dr. von Ziegler is a research fellow in cardiovascular imaging at the University of Florida at Jacksonville.
References
1. Halliburton SS, Petersilka M, Schvartzman PR, et al. Evaluation of left ventricular dysfunction using multiphasic reconstructions of coronary multi-slice computed tomography data in patients with chronic ischemic heart disease: validation against cine magnetic resonance imaging. Int J Cardiovasc Imaging 2003;19:73-78.
2. Grude M, Juergens KU, Wichter T, et. al. Evaluation of global left ventricular myocardial function with electrocardiogram-gated multidetector computed tomography: comparison with magnetic resonance imaging. Invest Radiol 2003;38:653-661.
3. Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultra-fast computed tomography. J Am Coll Cardiol 1990;15:827-832.
4. Arad Y, Goodman KJ, Roth M, et al. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol 2005;46:158-165.
5. Shaw LJ, Raggi P, Schisterman E, et al. Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality. Radiology 2003;228:826-833.
6. Greenland P, Smith SC, Grundy SM. Improving coronary heart disease risk assessment in asymptomatic people: role of traditional risk factors and non-invasive cardiovascular tests. Circulation 2001;104:1863-1867.
7. Achenbach S, Ropers D, Pohle FK, et al. Detection of coronary artery stenosis using multi-detector CT with 16x0.75 mm collimation and 375 ms rotation. Eur Heart J 2005;26:1978-1986.
8. Leber AW, Knez A, von Ziegler F, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography. A comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 2005;46:147-154.
9. Ropers D, Moshage W, Daniel WG, et al. Visualization of coronary artery anomalies and their course by contrast-enhanced electron beam tomography and three-dimensional reconstruction. Am J Cardiol 2001;87:193-197.
10. Datta J, White CS, Gilkeson RC, et al. Anomalous coronary arteries in adults: depiction at multi-detector row CT angiography. Radiology 2005;235-812-818.
11. Becker CR, Knez A, Ohnesorge B, et al. Imaging of noncalcified coronary plaques using helical CT with retrospective ECG gating. AJR 2000;175:423-424.
12. Leber AW, Knez A, Becker A, et al. Accuracy of multidetector spiral computed tomography in identifiying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am Coll Cardiol 2004;43:1241-1247.
13. Nieman K, Pattynama PMT, Rensing BJ, et al. Evaluation of patients after coronary artery bypass surgery: CT angiographic assessment of grafts and coronary arteries. Radiology 2003;229:749-756.
14. Gilard M, Comly JC, Rioufol G, et al. Noninvasive assessment of left main coronary stent patency with 16-slice computed tomography. Am J Cardiol 2005;95:110-112.
15. Schuijf JD, Bax JJ, Jukema JW, et al. Feasibility of assessment of coronary stent patency using 16-slice computed tomography. Am J Cardiol 2004;94:427-430.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.