CT Predicts Stroke Patients Benefitting From Endovascular Thrombectomy
When used together, non-contrast simple CT and CT perfusion have higher prediction rates
Computed tomography – both simple and advanced – can accurately predict which stroke patients will most likely benefit from endovascular thrombectomy to remove large cerebral clots. And, the predictive capability increases when both CT profiles are used together.
Results from the multi-center study, conducted by investigators at The University of Texas Health Science Center at Houston (UTHealth), were published recently in
Ischemic stroke, caused by an artery blockage, is the most common form of stroke. In most cases, endovascular thrombectomy – threading a mechanical device through the artery – can be an effective treatment that improves clinical outcomes up to 24 hours from onset.
Imaging is required to determine where the clot is located and whether the patient is a good thrombectomy candidate, meaning they have a smaller area of brain tissue death. According to Amrou Sarraj, M.D., lead author and associate professor of neurology at UTHealth’s McGovern Medical School, different imaging techniques are currently used to make this decision, but little is known about how they correlate with each other.
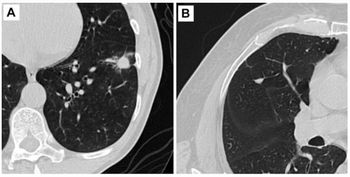
Both non-contrast simple CT and CT with injected contrast dye (CT perfusion) are routinely used to pinpoint the clot and the surrounding areas of cellular death. Most hospitals have access to simple CT, but CT perfusion is frequently only available at advanced stroke centers.
Investigators reviewed both the CT and CT perfusion results of 361 enrolled patients. Most had favorable imaging results on both types of scans, indicating they were strong candidates for endovascular thrombectomy. Additionally, those patients had significantly higher chances of receiving endovascular therapy, and 58 percent had better recovery rates after 90 days.
In cases where the imaging modalities disagreed, Sarraj said, functional and safety outcomes were still acceptable. Among patients, 38 percent reached functional independence, a higher amount than patients who didn’t receive thrombectomy. However, patients who had unfavorable CT perfusion results, but favorable simple CT ones, did experience more post-stroke symptomatic brain tissue hemorrhage and death. Patients with unfavorable results for both modalities had very poor outcomes.
An additional, ongoing trial is focused on assessing the safety and efficacy of thrombectomy procedures in patients with unfavorable profiles on one or both imaging modalities.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.














