Emerging research suggests that microstructural mapping with time-dependent diffusion magnetic resonance imaging (MRI) is not only effective at identifying molecular subtypes of breast cancer but also has the potential to predict patient response to neoadjuvant chemotherapy.
In the prospective study, recently published in Radiology, researchers reviewed data from 408 participants (mean age of 51.9) who had breast MRI prior to treatment for invasive breast cancer in order to compare time-dependent diffusion MRI to apparent diffusion coefficient (ADC) measurement for ascertaining molecular subtypes of breast cancer.
For 221 study participants who received neoadjuvant chemotherapy, the study authors also evaluated a model combining time-dependent diffusion MRI microstructural parameters with the factors of human epidermal growth factor receptor 2 (HER2) and progesterone receptor in comparison to standard diffusion-weighted MRI and clinical-pathologic models for the prediction of pathologic complete response (pCR), according to the study.
The researchers found that ADC measurements from conventional diffusion-weighted MRI (DWI MRI) exhibited a 73 percent area under the curve (AUC) for predicting pCR to neoadjuvant chemotherapy in contrast to 79 percent for a clinical-pathologic model that combined the progesterone receptor with HER2. However, the time-dependent diffusion MRI parameter of cellularity demonstrated the highest AUC at 84 percent, according to the study authors. The researchers said the AUC increased to 88 percent when cellularity was combined with clinical-pathologic characteristics.
The cellularity factor with time-dependent diffusion MRI also accounted for the highest AUC for predicting pCR to neoadjuvant chemotherapy in women with triple-negative breast cancer (TNBC) (92 percent), women with the luminal B subtype of breast cancer (78 percent) and those with the HER2-enriched subtype (74 percent).
“Cellularity was a crucial marker among time-dependent diffusion MRI microstructural parameters and showed the highest performance in predicting pCR,” wrote lead study author Xiaoxia Wang, M.D., who is affiliated with the Department of Radiology at the Chongqing University Cancer Hospital and the Chongqing Key Laboratory for Intelligent Oncology in Breast Cancer in Chongqing, China, and colleagues.
Three Key Takeaways
1. Predictive power of time-dependent diffusion MRI. Time-dependent diffusion MRI, particularly the cellularity parameter, showed the highest predictive accuracy (84 percent AUC) for determining the pathologic complete response (pCR) to neoadjuvant chemotherapy, outperforming standard ADC measurements and clinical-pathologic models.
2. Performance in subtypes. The cellularity parameter demonstrated high predictive accuracy for pCR across various breast cancer subtypes, achieving 92 percent AUC for triple-negative breast cancer (TNBC), 78 percent for luminal B, and 74 percent for HER2-enriched subtypes.
3. Subtype Identification. Time-dependent diffusion MRI microstructural mapping was more effective in identifying molecular subtypes of breast cancer (70-85 percent AUC range) than conventional methods like intravoxel incoherent motion or diffusion-kurtosis imaging, making it a valuable tool for subtype characterization.
The researchers also determined that time-dependent diffusion MRI microstructural mapping had a higher AUC range overall for determining molecular subtypes of breast cancer (70 to 85 percent) in contrast to that of intravoxel incoherent motion (60 percent to 86 percent) and diffusion-kurtosis imaging (50 percent to 78 percent) obtained with DWI MRI.
“In our study, time-dependent diffusion MRI microstructural parameters demonstrated excellent performance in helping to identify four molecular subtypes … , which was better than that of the apparent diffusion coefficient parameters derived from diffusion-weighted imaging,” noted Wang and colleagues.
(Editor’s note: For related content, see “Can DWI MRI Offer a Viable Non-Contrast Alternative for Breast Cancer Assessment?,” “Enhancing Lesions on Breast MRI: Can an Updated Kaiser Scoring Model Improve Detection?” and “Breast MRI Study Examines Common Factors with False Negatives and False Positives.”)
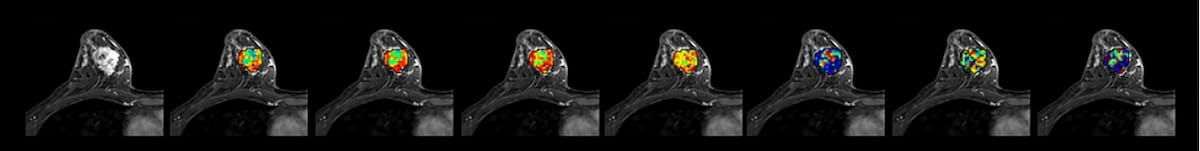
Beyond the inherent limitations of a single-center exploratory study, the authors acknowledged manual definition of tumor regions of interest. They also conceded that the use of average time-dependent diffusion MRI microstructure parameters for tumor regions of interest did not take intratumoral heterogeneity into account. The study authors also pointed out that the potential for variability between pulsed gradient spin echo and oscillating gradient spin echo MRI sequences due to intravoxel incoherent motion effects.