Emerging research on mammography screening suggests that premenopausal Asian and Pacific Islander women and postmenopausal Black women have the highest breast density-related risk and highest BMI-related risk, respectively, for developing advanced breast cancer. The researchers also found that mammography screening interval (annual versus biennial) had little impact on advanced breast cancer risk.
For the study, recently published in JAMA Oncology, researchers assessed population attributable risk proportions (PARPs) for advanced breast cancer based upon their review of data from 904,615 women who had a total of 3,331,740 annual or biennial mammography exams between January 2005 to June 2018. Seventy-two percent of the mammography exams were for White women with 10.8 percent for Asian or Pacific Islander women, 9.5 percent for Black women, 5.3 percent for Hispanic/Latinx women and 2 percent for women of other races and ethnicities, according to the study.
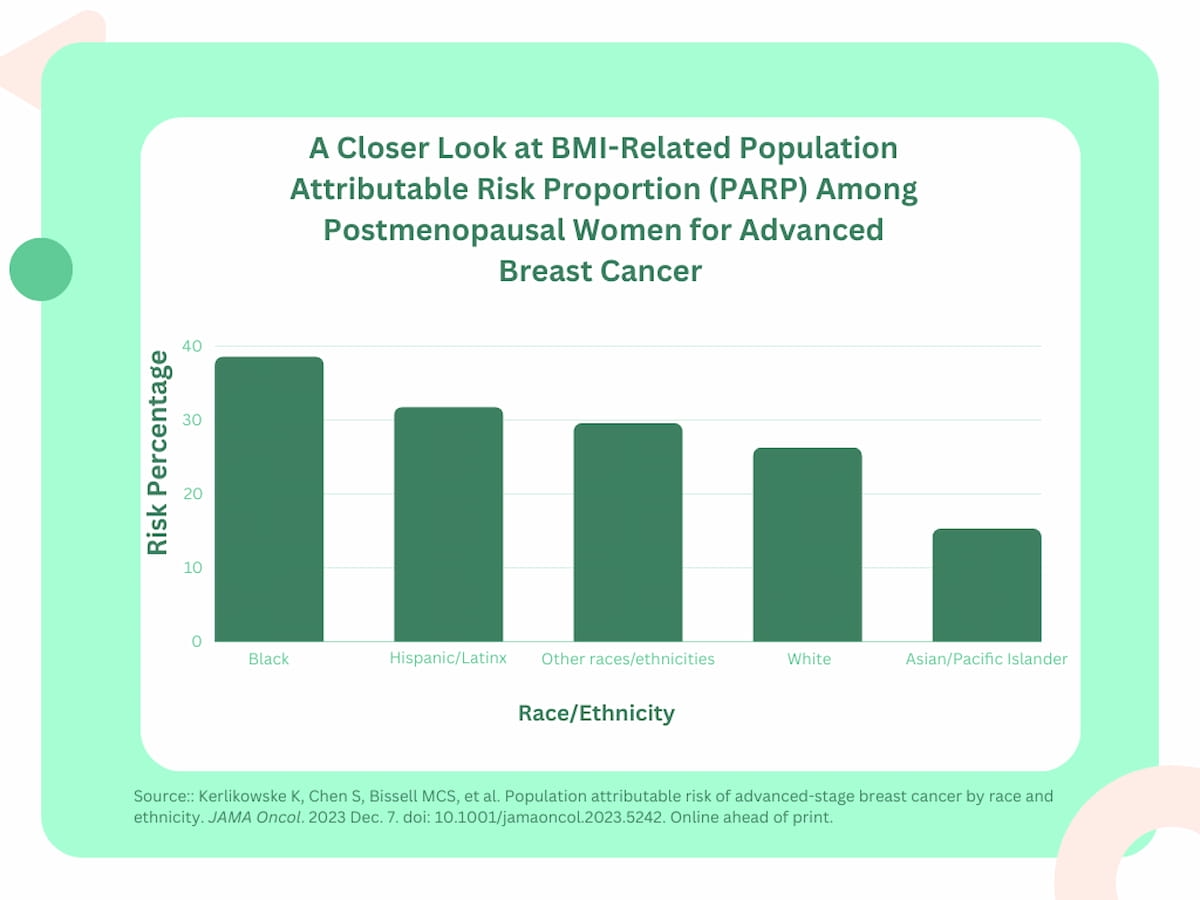
The researchers found that postmenopausal Black women had the highest body mass index (BMI)-related PARP (38.6 percent) for advanced breast cancer, followed by postmenopausal Hispanic/Latinx women (31.8 percent) and premenopausal Black women (30.3 percent). Postmenopausal and premenopausal Asian or Pacific Islander women had the lowest BMI-related PARP in the study at 15.3 percent and 9.8 percent respectively.
Being overweight or obese significantly increased PARPs for advanced breast cancer in contrast to invasive breast cancer for premenopausal women, according to the study authors. In this population, Black women had a 30.3 percent PARP for advanced breast cancer in comparison to a 9.9 percent PARP for invasive breast cancer. Similarly, the researchers also noted over a 20-fold higher PARP difference among Hispanic/Latinx women (23.4 percent vs. 1 percent) and White women (18.2 percent vs. 3.7 percent).
“(Being overweight or obese) accounted for the largest proportion of advanced cancers in postmenopausal women (30%) … . To reduce the number of advanced cancer diagnoses, primary prevention interventions should focus on shifting patients with overweight (status) and obesity to normal weight,” wrote lead study author Karla Kerlikowske, M.D., a professor of medicine at the University of California, San Francisco (UCSF) School of Medicine, and colleagues.
Breast density-related PARP was higher among premenopausal women (37 percent) overall in comparison to postmenopausal women (24 percent). Among premenopausal women, the study authors found that Asian or Pacific Islander women had the highest breast density-related PARP for advanced breast cancer (46.6 percent), followed by women of other races/ethnicities (40.2 percent) and White women (39.8 percent).
Kerlikowske and colleagues noted that factors such as alcohol intake, postmenopausal estrogen and progesterone therapy may contribute to increased breast density. The study authors added that selective estrogen receptor modulators, gonadotropin-releasing hormone agonists and breast feeding can lead to decreases in breast density.
Three Key Takeaways
- Breast density-related risk in premenopausal Asian and Pacific Islander women. Premenopausal Asian and Pacific Islander women were found to have the highest breast density-related risk for developing advanced breast cancer, with a breast density-related population attributable risk proportion (PARP) of 46.6 percent. This underscores the importance of considering breast density as a significant factor in assessing breast cancer risk among premenopausal women of specific ethnic backgrounds.
- BMI-related risk in postmenopausal Black women. Postmenopausal Black women demonstrated the highest body mass index (BMI)-related PARP for advanced breast cancer, accounting for 38.6 percent. This highlights the critical role of BMI in assessing breast cancer risk in postmenopausal Black women. The study suggests that interventions to reduce advanced cancer diagnoses should focus on addressing overweight and obesity in this population.
- Impact of mammography screening interval on advanced breast cancer risk. The study found that the mammography screening interval (annual versus biennial) had little impact on advanced breast cancer risk, with screening intervals accounting for only a small proportion (2.1 to 2.3 percent) of advanced breast cancers. This suggests that factors such as breast density and BMI may have a more substantial influence on advanced breast cancer risk than the frequency of mammography screening.
“Notably, longitudinal decreases in breast density over time have been associated with reductions in breast cancer risk,” noted Kerlikowske and colleagues.
(Editor’s note: For related content, see “Should Race and Ethnicity Factor into Starting Ages for Mammography Screening?,” “The Reading Room Podcast: Emerging Concepts in Breast Cancer Screening and Health Equity Implications, Part 2” and “Study: Regular Mammography Screening Reduces Breast Cancer Mortality Risk by More than 70 Percent.”)
The researchers also pointed out that mammography screening interval (annual vs. biennial) related PARPs across pre- and postmenopausal women ranged between 2.1 to 2.3 percent.
“ … Biennial vs. annual screening accounted for only a small proportion of advanced breast cancers, a surrogate for breast cancer mortality,” said Kerlikowske and colleagues.
Other factors such as family history of breast cancer and breast biopsy history also had small PARPs for advanced breast cancer, according to the researchers, who noted a 5 to 8 percent PARP for family history and a 7 to 12 percent PARP for previous breast biopsy.
In regard to study limitations, the authors acknowledged that stratification by race, ethnicity and menopausal status resulted in smaller sample sizes and wider estimated confidence intervals. The researchers maintained there is no current evidence linking a decrease in advanced cancer risk to decreases in BMI and breast density. The study authors also acknowledged that the research may not be inclusive of all ethnic and racial groups in the United States.