MRI Study: Half-Dose Gadopiclenol Offers Similar Visualization and Safety as Full-Dose Gadobutrol
Newly published research suggests the use of gadopiclenol at 0.05 mmol/kg is non-inferior to gadobutrol 0.1 mmol/kg for all qualitative visualization parameters on full-body magnetic resonance imaging (MRI).
For full-body magnetic resonance imaging (MRI) exams, emerging research shows that clinicians can utilize a half-dose of the contrast agent gadopiclenol as opposed to a full dose of gadobutrol without any decline in visualization of lesions.
For the randomized multicenter phase 3 study, recently published in Radiology, researchers compared gadopiclenol at 0.05 mmol/kg dosing versus gadobutrol at 0.1 mmol/kg dosing in 260 patients who had two contrast-enhanced MRI examinations. According to the study, all patients had at least one focal lesion in one of three areas including: the musculoskeletal system; head and neck; or breast, thorax, abdomen, or pelvis.
In regard to lesion visualization, the study authors found no significant differences between the two contrast agents in border delineation, internal morphologic characteristics, and contrast enhancement. For the majority of the cohort (ranging from 75 to 83 percent), the three reviewing radiologists expressed no preference for gadopiclenol or gadobutrol, according to the researchers.
“Gadopiclenol at half the standard dose provided the same results as gadobutrol at the standard dose in terms of lesion visualization and overall image quality,” wrote study co-author Pamela M. Otto, M.D., F.A.C.R, who is affiliated with the Department of Radiology at the University of Texas Health Science Center at San Antonio in Texas, and colleagues.
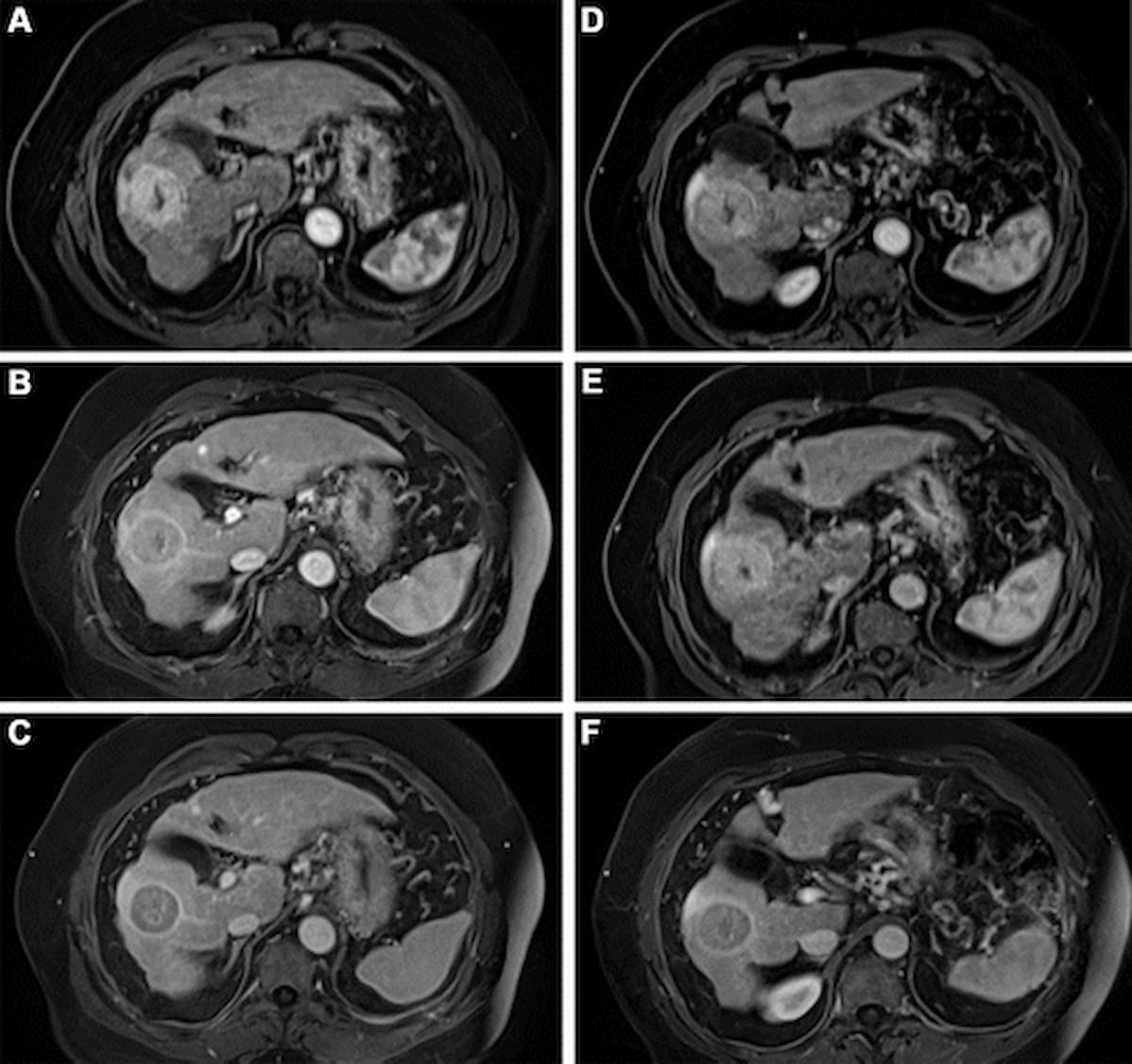
One can see contrast-enhanced MRI views of the liver for a 66-year-old man with hepatocellular carcinoma. The images in A-C were obtained with gadopiclenol 0.05 mmol/kg and the images in D-F were obtained with gadobutrol 0.1 mmol/kg gadobutrol. (Images courtesy of Radiology.)
(Editor’s note: For related content, see “FDA Approves New MRI Contrast Agent Gadopiclenol” and “A Closer Look at Ultrasound and MRI Alternatives for Head and Neck Imaging.”)
The study authors also noted a similar safety profile for both contrast agents. Eighteen percent of patients who had gadopiclenol had post-injection adverse events in comparison to 20 percent for those who had gadobutrol. The researchers noted that most of the reported adverse events were mild for both agents (74 percent for gadopiclenol and 77 percent for gadobutrol).
“The high stability of gadopiclenol, combined with its higher relaxivity and thus lower injected dose is expected to make it an attractive (gadolinium-based contrast agent), particularly for patients, who, based on their known disease or risk profile, are expected to undergo repeated contrast-enhanced MRI examinations, such as hepatic MRI for the surveillance of patients with liver cirrhosis or cerebral MRI for patients with multiple sclerosis,” emphasized Otto and colleagues.
In regard to study limitations, the researchers noted they did not assess sensitivity nor specificity of either contrast agent. Due to low numbers of participants in individual subgroups, the study authors emphasized caution with interpretation of results in these groups.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.