PET/CT or mpMRI: Which is Better for Detecting Biochemical Recurrence of Prostate Cancer?
A recent meta-analysis found that multiparametric MRI and PET/CT had comparable detection rates for diagnosing prostate cancer recurrence.
Positron emission tomography/computed tomography (PET/CT) and multiparametric magnetic resonance imaging (mpMRI) offer similar detection rates for diagnosing prostate cancer (PCa) recurrence, according to a recent meta-analysis.
For the systematic review, recently published in Clinical Radiology, researchers reviewed six studies comparing the use of PET/CT and mpMRI in diagnosing PCa. The combined cohort was comprised of 290 patients who had biochemical recurrence (BCR) of PCa, according to the meta-analysis.
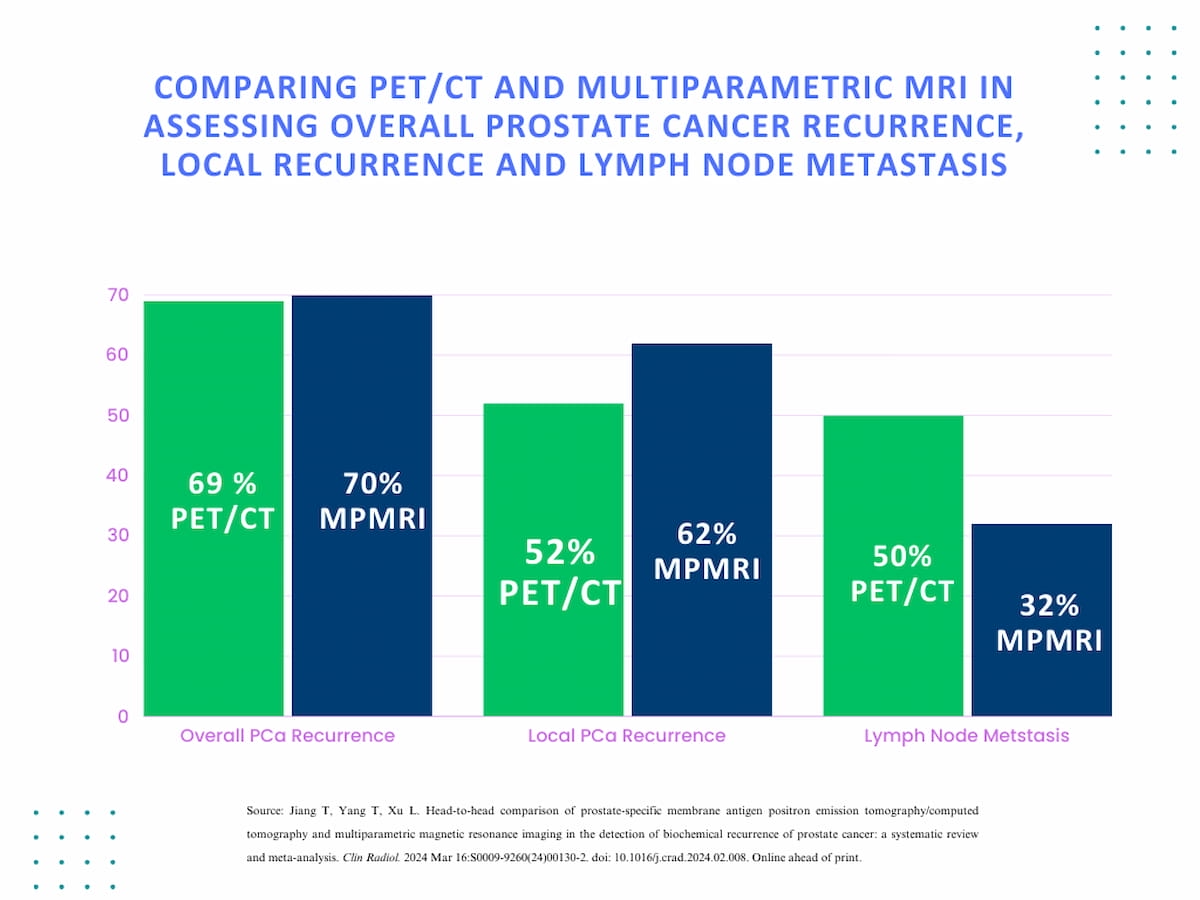
The researchers found that prostate-specific membrane antigen (PSMA) PET/CT had a pooled overall detection rate of 69 percent for PCa recurrence in comparison to 70 percent for mpMRI.
The researchers found that prostate-specific membrane antigen (PSMA) PET/CT had a pooled overall detection rate of 69 percent for PCa recurrence in comparison to 70 percent for mpMRI. They also noted that differences between the two modalities with respect to local PCa recurrence and lymph node metastasis detection were not statistically significant.
“When it comes to (biochemical recurrence), both methods work effectively. Our findings indicated no discernible difference in the overall DRs (detection rates) of the two imaging modalities, with mpMRI being more cost-effective while maintaining the same DR,” wrote study co-author L. Xu, who is affiliated with the Medical School at the Hunan University of Chinese Medicine in Hunan, China, and colleagues.
For local PCa recurrence, the study authors noted a 10 percent higher DR for mpMRI (62 percent vs. 52 percent). The researchers also found a 18 percent higher DR for PSMA PET/CT in diagnosing lymph node metastasis (50 percent vs. 32 percent). However, neither of these findings had statistical significance, according to the study authors.
The researchers suggested that high sensitivity and specificity may make PSMA PET/CT more advantageous for staging PCa and in detecting smaller lesions but acknowledged that availability of the modality is an issue. Multiparametric MRI may provide benefits in diagnosing local recurrence and clinically significant PCa, but the study authors conceded that interobserver heterogeneity can be an issue with mpMRI.
However, the overall findings from the meta-analysis suggested that both modalities have a role in diagnosing PCa BCR and noted that future prospective studies could provide more clarity in this regard.
“The study's findings have significant ramifications for clinical practice. The same diagnostic performance of PSMA PET/CT and mpMRI shows that both techniques can successfully identify BCR in patients with PCa. To assess the affordability, accessibility, and cost-effectiveness of these imaging modalities, more research is nonetheless required,” maintained Xu and colleagues.
In regard to study limitations, the authors acknowledged the small sample size of 290 total patients due to the emphasis on reviewing comparative studies for detection of BCR in the same patient cohorts. They also suggested possible bias with the results given the variety of imaging protocols and patient characteristics in the six reviewed studies.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.
The Reading Room Podcast: Current Perspectives on the Updated Appropriate Use Criteria for Brain PET
March 18th 2025In a new podcast, Satoshi Minoshima, M.D., Ph.D., and James Williams, Ph.D., share their insights on the recently updated appropriate use criteria for amyloid PET and tau PET in patients with mild cognitive impairment.