Quantitative MRI Scanner Measurements Vary
Study from NIST shows great variation between MRI scanners from multiple vendors, limiting accuracy and diagnostic confidence.
Quantitative MRI does a better job with disease detection and diagnosis, but greater levels of quality control are needed to maximize its abilities.
In a study published Wednesday in PLOS One, investigators from the National Institute of Standards and Technology (NIST), examined measurement variations in these scanners that offer greater accuracy, repeatability, and speed.
“We suggest establishing rigorous quality control procedures for quantitative MRI to promote confidence and stability in associated measurement techniques and to enable translation of measurement thresholds for diagnostic, disease progression, and treatment monitoring from the research center to the entire clinical community and back,” said the team led by Katy Keenan, Ph.D., NIST’s Quantitative Magnetic Resonance Imaging Project leader.
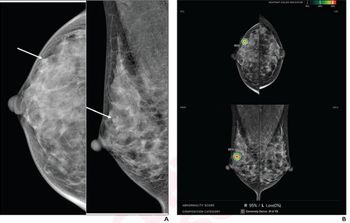
Quantitative MRI has been heralded as a way to provide consistent disease detection, diagnosis, and treatment without the need of a tissue biopsy. It outpaces traditional MRI, the team said, as conventional methods can produce subjective image analysis and contradictory images. For quantitative MRI to be truly reliable, though, the numerical measurements it captures should be consistent across different patients, scanners, and clinical environments.
To test that consistency, the NIST team, which included investigators from 11 institutions, compared measurements captured by 27 MRI scanners produced by three vendors (GE Healthcare, Siemens Healthineers, and Philips) at nine clinical sites. They used a NIST-produced phantom for the scans to obtain reference values and disentangle any sources of bias, they said.
The team compared T1 measurements across scanners – it’s one of the parameters that could be measured by clinical MRI systems. However, they determined that these values can be subject to significant bias and variation. From their analysis, there was no consistent pattern of discrepancy between vendors, meaning that the diagnostic threshold value determined on one MRI scanner can’t transfer to other systems, they said.
Consequently, they said, it is possible that such a variation could make a clinical difference and affect patient care, such as misdiagnosing a benign or malignant brain tumor.
Ultimately, they said, rigorous quality control procedures could lead to greater confidence and measurement stability. It could also make it easier to transfer measurement threshold for diagnosis, disease progression, and treatment monitoring between research and clinical venues.
For more coverage based on industry expert insights and research, subscribe to the Diagnostic Imaging e-Newsletter
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.