Study Confirms Higher Accuracy of MRI Over Emerging PSMA PET/CT for Diagnosing Prostate Cancer
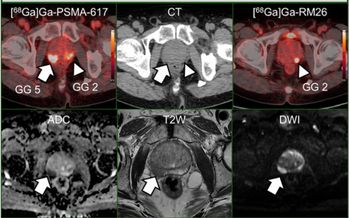
Magnetic resonance imaging (MRI) had better accuracy than prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) “for detecting any grade of prostate cancer,” according to new study findings presented at the European Association of Urology Annual Congress (EAU22) in Amsterdam.
Magnetic resonance imaging (MRI) continues to be the “gold standard of pre-biopsy detection” for prostate cancer, according to the authors of a new study that compared MRI to the use of prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT).
In the phase III multicenter study involving 240 patients at risk for prostate cancer, each patient had MRI and PSMA PET/CT scans. The study authors, who presented their findings at the recent European Association of Urology Annual Congress, noted that PSMA PET/CT detected abnormalities in 198 patients while MRI scans revealed abnormalities in 141 patients.
After reviewing results for 181 patients who had a prostate biopsy, the researchers found that MRI had a 75 percent accuracy rate for detecting prostate cancer in comparison to a 62 percent accuracy rate for PSMA PET/CT.
“Our analysis found that MRI scans were better than PSMA-PET for detecting any grade of prostate cancer,” noted study co-author Lih-Ming Wong, MD, an associate professor in the Department of Surgery at the University of Melbourne and a consultant uro-oncologist at St. Vincent’s Hospital in Melbourne, Australia.
However, Dr. Wong noted that when the researchers looked only at the detection of clinically significant prostate cancer, there was no difference in accuracy between the two imaging modalities. He added that detection thresholds may be tweaked moving forward as researchers are just starting to assess the diagnostic utility of PSMA PET/CT for prostate cancer.
While Dr. Wong doesn’t see PSMA PET/CT supplanting MRI, he noted that it could potentially have adjunctive diagnostic value for patients at risk for prostate cancer.
“This study confirms that the existing ‘gold standard’ of pre-biopsy detection — the MRI — is indeed a high benchmark,” explained Dr. Wong. “Even with fine-tuning, we suspect PSMA PET/CT won’t replace MRI as the main method of prostate cancer detection. But it likely will have application in the future as an adjunct to the MRI, or for people for whom an MRI is unsuitable, or as a single combined ‘diagnostic and staging’ scan for appropriately selected patients.”
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.