Tomosynthesis cuts breast screening callbacks, boosts detection
Breast tomosynthesis used in the screening setting detects more breast masses, better categorizes those masses, and produces lower callback rates than conventional mammography, according to research presented at the RSNA meeting. Tomosynthesis was not superior to mammography in one study of symptomatic patients, but a combination of the two techniques detected more carcinomas than either alone.
Breast tomosynthesis used in the screening setting detects more breast masses, better categorizes those masses, and produces lower callback rates than conventional mammography, according to research presented at the RSNA meeting. Tomosynthesis was not superior to mammography in one study of symptomatic patients, but a combination of the two techniques detected more carcinomas than either alone.
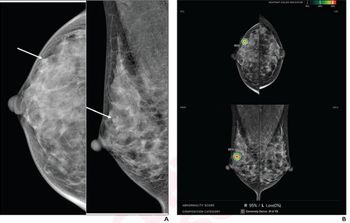
Citing results gathered from 30 subjects in an ongoing study, Dr. Mark A. Helvie, director of breast imaging at the University of Michigan Health System, reported that experienced readers detected more masses using tomosynthesis, a 3D digital mammography technique, than with conventional 2D mammography. Tomosynthesis provided better margin assessment and malignant characterization, and it identified cancer that was hidden on mammography.
Helvie reported that 100% of cancers were detected using tomosynthesis, compared with 83% using mammography. Average results from three experienced readers showed that 36% more masses were found by tomosynthesis, which visualized 48% more margin than mammography. Malignant cases were rated as 48% more likely to be malignant on tomosynthesis compared with mammography, while benign cases had the same malignancy rating (18%).
In a late-breaking RSNA paper, Dr. Elizabeth Rafferty, director of breast imaging at Massachusetts General Hospital, presented results from a multicenter, multireader trial assessing the value of tomosynthesis as an adjunct to full-field digital mammography. The trial was conducted at five clinical sites: Massachusetts General: University of Iowa; Yale; Dartmouth Hitchcock Medical Center; and Magee-Women's Hospital at the University of Pittsburgh.
The study included 1083 women, 856 of whom presented for screening and 227 for breast biopsy. Twelve radiologists scored FFDM images, then reviewed FFDM with tomosynthesis. Combined readings resulted in an increase in sensitivity from 65.5% to 76.2%. Specificity increased from 84.1% to 89.2%, and the recall rate was cut from 51.5% to 12.9%, a 38.6% decrease.
Similarly, tomosynthesis significantly reduced callback rates in an ongoing screening trial sponsored by the National Cancer Institute, according to Richard Moore, director of breast imaging research at Mass General. Patients who had prior studies and were then imaged using tomosynthesis had a callback rate of 5.1%, 25.1% lower than the baseline radiologist rate of 6.8% and 37% lower than the average mammography rate of 8%. Available prior studies reduced callback rates about 5% for both mammography and tomosynthesis.
The research compared 2233 mammography screening studies performed on 2115 women with 2233 tomosynthesis studies performed on 2114 women between June 2005 and September 2007. Both types of studies were read in batch mode.
Among patients with no prior studies, the callback rate was 12.9% for mammography and 11.6% for tomosynthesis. For patients with prior studies, rates were 8.1% and 5.1%, respectively.
The research also suggested that the tomosynthesis callback rate improves with experience. In the first eight months the system was in use, the callback rate was 6.3% for patients who had received prior studies. In the third eight-month period, that rate dropped to 4.5%.
Moore warned that the appearance of previous surgery on tomosynthesis can be jarring when radiologists first begin using the system, as a surgical scar can mimic a new lesion.
Results from another study threw some cold water on the tomosynthesis lovefest, however. Dr. Hendrik Teertstra of the Netherlands Cancer Institute in Amsterdam presented research suggesting that the ability to detect malignant lesions was not significantly different for tomosynthesis and mammography and that the role of tomosynthesis has yet to be established in symptomatic patients. A combination of the two techniques did detect more carcinomas than either technique alone.
The study of 113 carcinomas in 933 symptomatic breasts determined that the rate of false negatives produced using tomosynthesis was 6.2%, while that using mammography was 7%. Using a combination of the two techniques, false negatives dropped to 2.65%.
For more information from the Diagnostic Imaging archives:
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.














