An absent hilum on ultrasound (US) imaging is 169.7 times more likely to be associated with three or more metastatic axillary lymph nodes (ALNs) in women with T1-2N0 breast cancer, according to new research.
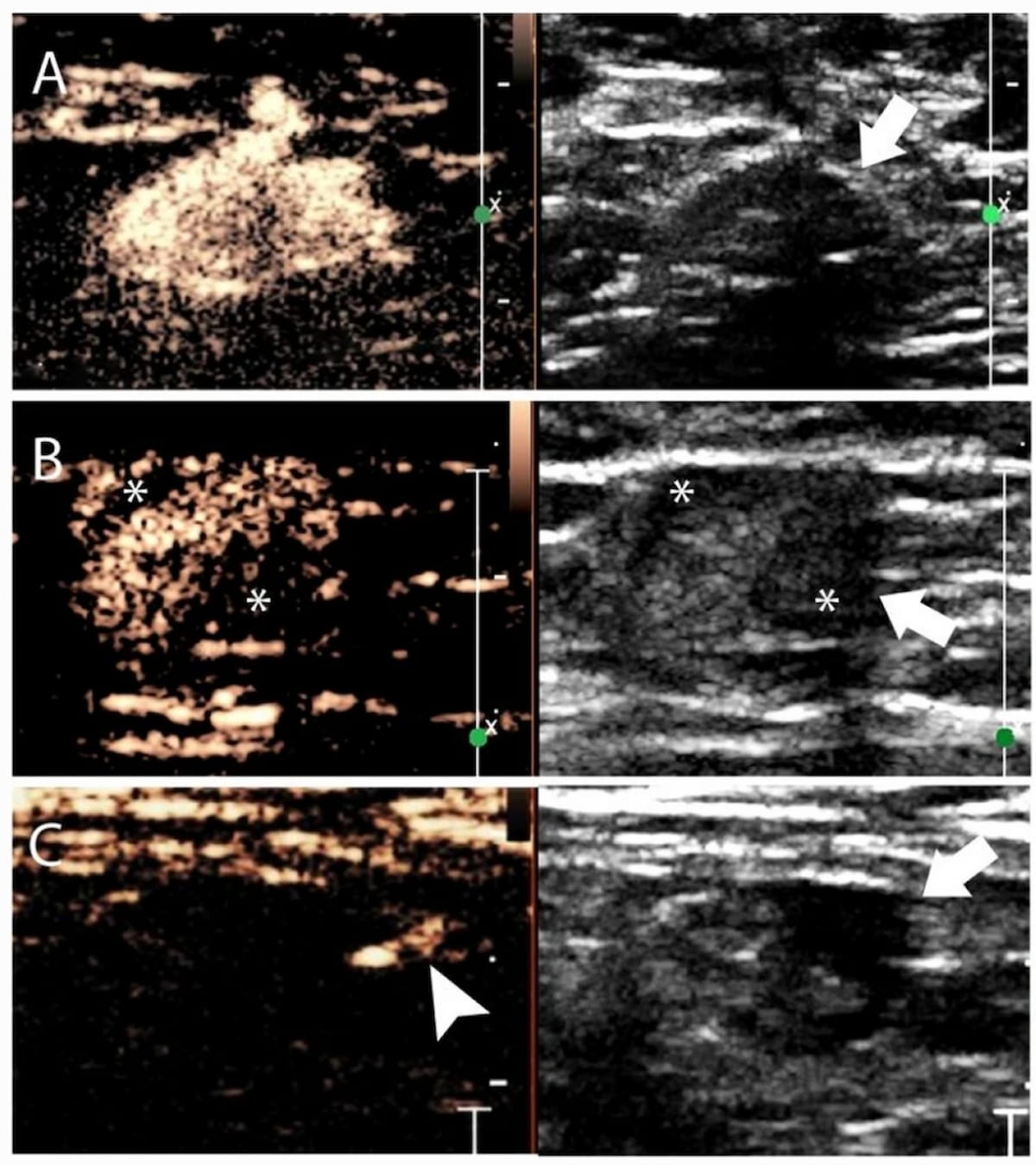
For the multicenter prospective study, recently published in Insights into Imaging, researchers reviewed contrast-enhanced (CE) lymphatic US images, grayscale US scans and clinicopathologic data from women with T1-2N0 breast cancer. The creation of a nomogram that combines these findings for the preoperative prediction of metastatic ALNs was developed with 179 patients, internally validated with 90 patients, and underwent external validation testing in a group of 197 women, according to the study.
Multivariate analysis revealed that sentinel lymph nodes (SLNs) with no enhancement on US were 15.3 times more likely to be associated with three or more metastatic ALNs in women with T1-2N0 breast cancer. The researchers also noted three cortical morphology findings on US that were independently associated with three or more metastatic ALNs in this patient population. These findings included a 19.1 odds ratio (OR) for diffuse cortical thickening, a 27.7 OR for focal eccentric cortical thickening and a 169.7 OR for an absent hilum.
For the prediction of three or more metastatic ALNs, the study authors found that the nomogram provided a 10 percent higher sensitivity rate than grayscale US alone (33.3 percent vs. 23.5 percent) but four percent lower than that of lymphatic US alone (37.3 percent. While the nomogram had comparable specificity and accuracy to grayscale and lymphatic US use alone, researchers said the nomogram offered a higher positive predictive value (68 percent vs. 63.2 percent for grayscale US and 55.9 percent for lymphatic US) and a higher area under the curve (AUC) (88 percent vs. 83 percent for grayscale US and 79 percent for lymphatic US).
“The nomogram based on conventional US and CE lymphatic US was demonstrated to be feasible for the ALN staging. … By setting the threshold at 40%, we achieved the highest positive predicted value, thus minimizing over-treatment of patients with low metastatic burden,” wrote study co-author Qingli Zhu, M.D., who is affiliated with the Department of Ultrasound at the Peking Union Medical College and Peking Union Medical College Hospital in Beijing, China, and colleagues.
Three Key Takeaways
- Significance of absent hilum on ultrasound. An absent hilum on ultrasound imaging is strongly associated with a higher likelihood of three or more metastatic axillary lymph nodes (ALNs) in women with T1-2N0 breast cancer, with an odds ratio of 169.7. This finding underscores the importance of careful ultrasound examination for identifying potential metastatic involvement in breast cancer staging.
- Utility of nomogram in predicting metastatic ALNs. The development of a nomogram combining conventional ultrasound and contrast-enhanced lymphatic ultrasound findings offers improved sensitivity (33.3 percent) compared to grayscale ultrasound alone (23.5 percent) for predicting three or more metastatic ALNs. While maintaining comparable specificity and accuracy, the nomogram demonstrates a higher positive predictive value (68 percent) and a higher area under the curve (AUC) (88 percent), highlighting its potential as a preoperative tool for ALN staging.
- Considerations for nomogram sensitivity. Despite its potential as a preoperative tool for axillary lymph node (ALN) staging in breast cancer, the nomogram developed in this study exhibits a low sensitivity rate. Clinicians should be cautious about relying solely on the nomogram for identifying patients with high tumor burden in ALNs. Standard sentinel lymph node (SLN) biopsy remains crucial to prevent missed diagnoses in these cases, emphasizing the importance of combining clinical judgment with imaging findings for comprehensive patient management.
The study authors noted that factors including lymphovascular invasion as well as tumor size, grade and type are factors to consider with the development of ALNs. However, they emphasized that US findings were the only findings that correlated with three or more metastatic ALNs.
“Although there were several differences in the clinical and histopathological variables between the development and validation groups, our nomogram showed similar specificity and accuracy in the two cohorts and appears to be a robust tool to provide preoperative information,” maintained Zhu and colleagues.
Acknowledging the low sensitivity rate of the nomogram, the researchers maintained that standard SLN biopsy could prevent missed diagnoses of patients with high tumor burden. However, they conceded the potential for false positive cases given that inhomogeneous enhancement and non-enhancement on lymphatic US with SLNs can occur regardless of the degree of metastatic burden with ALNs. The study authors suggested the combination of radiomics and CE lymphatic US images of SLN could enhance diagnostic accuracy for these cases in the future.
(Editor’s note: For related content, see “AI and Breast Ultrasound: Where Things Stand,” “Can AI Rein in Follow-Up Exams and Benign Lesion Biopsies After Breast Ultrasound?” and “Whole Breast Ultrasound Screening: Is There Adequate Utilization in Patients at Higher Risk for Breast Cancer?”)
In regard to study limitations, the authors conceded that there is a learning curve for assessing contrast-enhanced (CE) lymphatic ultrasound. The researchers also acknowledged that prior biopsy procedures can affect the viewing of lymphatic vessels and that the study only included one SLN diagnosed with CE lymphatic ultrasound.