Use of the Ovarian-Adnexal Imaging Reporting and Data System (O-RADS) ultrasound (US) risk score may prevent unnecessary surgery for a significant number of women with ovarian cystic lesions and no acute symptom presentation, according to findings from a new multicenter study.
For the retrospective study, recently published in Radiology, researchers reviewed pre-op ultrasound imaging from 377 patients (median age of 45) with ovarian cystic lesions and non-acute symptoms who underwent surgical resection between January 2011 and December 2014.
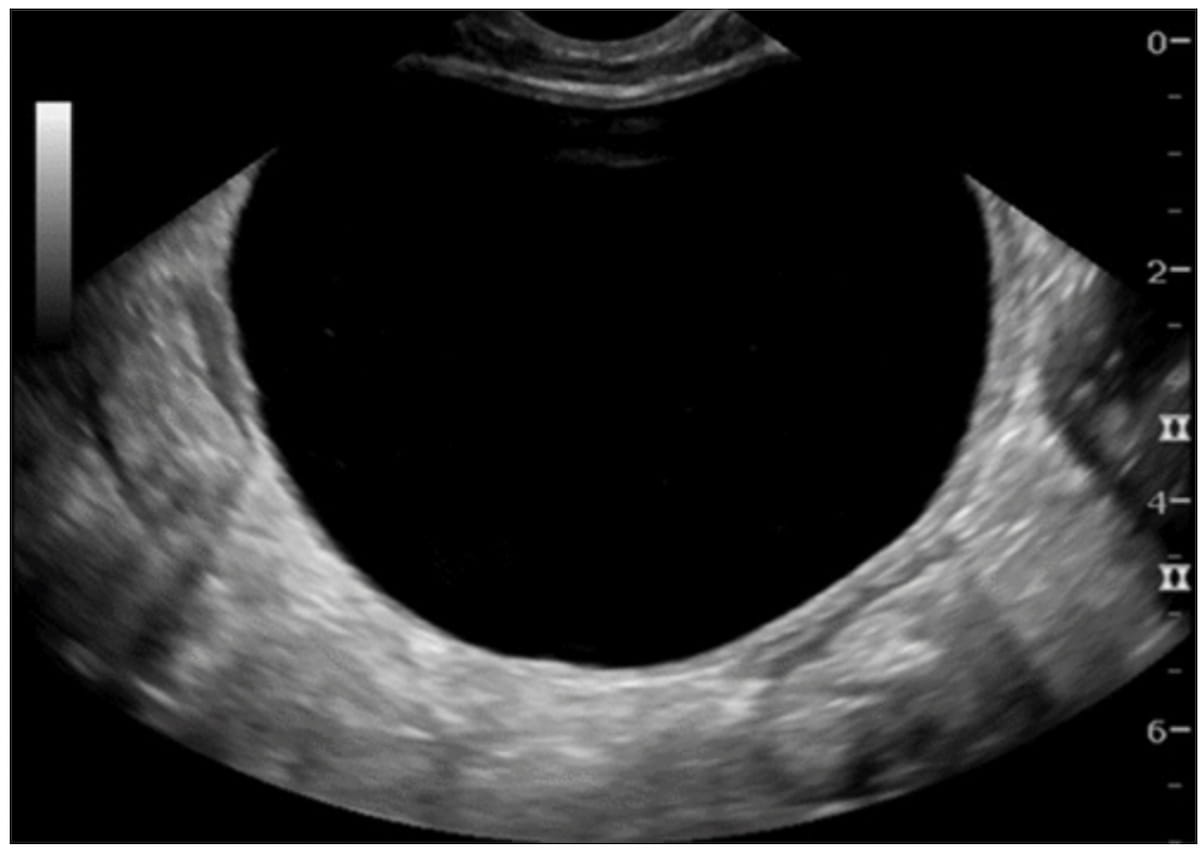
The researchers found that 157 of the resected lesions (42 percent) would have been classified with an O-RADS US 2022 risk score of 2. The study authors noted that 86 of these lesions (54 percent) were non-neoplastic and 70 lesions (45 percent) were dermoids or other benign tumors.
“If the O-RADS US version 2022 risk stratification system had been used in this patient population, lesions in nearly half of the patients would have been scored as O-RADS US 2, and these patients could have been offered follow-up imaging or conservative treatment,” wrote lead study author Luyao Shen, M.D., who is affiliated with the Department of Radiology at the Stanford University School of Medicine in Stanford, Calif., and colleagues.
The study authors also found that employing an O-RADS US 4 score as a minimum threshold for detection of malignancy yielded a 94 percent sensitivity rate and a 98 percent negative predictive value (NPV).
While noting the high reliability of the O-RADS US risk scoring system for excluding malignant diagnoses, the researchers cautioned that the O-RADS US system has drawbacks in specificity (64 percent) and positive predictive value (PVV) (38 percent).
“This decreased specificity and PPV limit the use of O-RADS US version 2022 for predicting the presence of malignancy in this patient population,” noted Shen and colleagues.
Three Key Takeaways
1. Potential to reduce unnecessary surgery. Use of the O-RADS US 2022 risk stratification system could have prevented surgery in nearly half of the studied patients with ovarian cystic lesions, offering them follow-up imaging or conservative management instead.
2. High sensitivity and NPV for malignancy. Employing an O-RADS US 4 score as the minimum threshold for malignancy detection yielded a 94 percent sensitivity and a 98 percent negative predictive value (NPV), demonstrating its reliability in ruling out malignant ovarian lesions.
3. Limitations in specificity. While O-RADS US is reliable in excluding malignancy, its lower specificity (64 percent) and positive predictive value (38 percent) limit its accuracy in predicting malignancy. MRI may be useful for further characterization of uniocular cysts scored as O-RADS US 2 and lesions scored as O-RADS US 3 or higher..
In an accompanying editorial, Laure S. Fournier, M.D., Ph.D., praised the originality of the study in assessing the practical application and role of the O-RADS US system within the management of patients with ovarian and adnexal lesions.
In regard to the lower specificity of O-RADS US, Fournier said subsequent magnetic resonance imaging (MRI) can enhance characterization of uniocular cysts scored as O-RADS US 2 as well as other lesions with O-RADS US 3 or higher risk scores.
“Moreover, MRI allows for identification of certain histologic types, which helps the surgeon know what to expect, prepare the procedure, and inform the patient on the possible findings,” added Dr. Fournier, a professor in the Department of Radiology at the Georges Pompidou European Hospital in Paris, France.
(Editor’s note: For related content, see “Key Challenges with the O-RADS Ultrasound Classification System,” “Is MRI More Effective than Ultrasound for Diagnosing Adnexal Lesions?” and “MRI or Ultrasound for Evaluating Pelvic Endometriosis?: Seven Takeaways from a New Literature Review.”)
In regard to study limitations, the authors noted the exclusion of patients with acute presentations at the time of ultrasound examination but still acknowledged possible patient selection bias with the likelihood of a higher PPV in a cohort of patients undergoing surgery. The researchers also noted that ultrasound scans were obtained by technologists who lacked training in gynecologic imaging and reviewed by radiologists in academic settings in contrast to non-academic practices where physicians with gynecologic imaging experience perform and interpret the scans.