Comparing resected pure ground-glass nodules (pGGNs) to part-solid nodules (PSNs) and heterogeneous ground-glass nodules (GGNs) in a new lung CT study, researchers found that those with resected pGGNs had very low recurrence rates up to seven years after treatment.
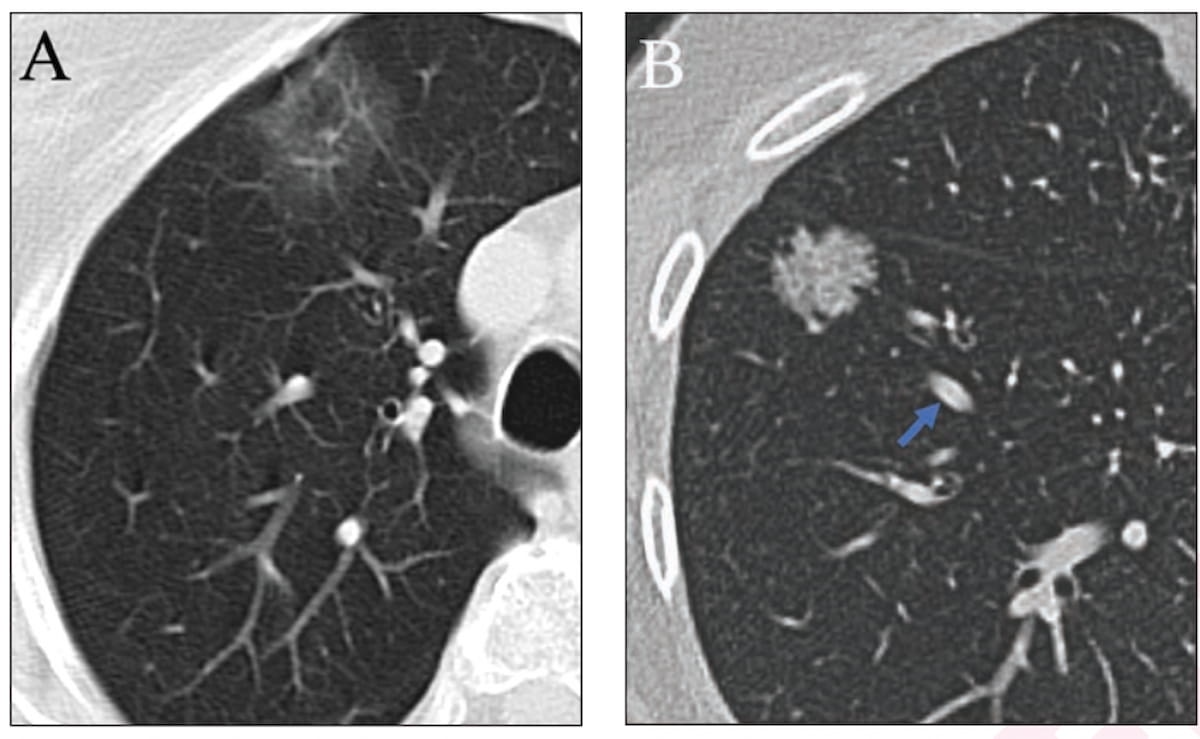
For the retrospective study, recently published in the American Journal of Roentgenology, researchers assessed clinical outcomes between 301 patients with PSNs (nodules with an internal solid component equal in density to pulmonary vessels), 109 patients with heterogeneous GGNs (described as nodules with increased internal density but not quite as dense as pulmonary vessels) and 59 patients with pGGNs (described as nodules with homogeneous ground-glass attenuation but no internal decrease in density).
The study authors found that those with pGGNs had a significantly lower frequency of invasive adenocarcinoma (39 percent) in comparison to patients with heterogeneous GGNs (67.9 percent) or PSNs (75.7 percent).
The patients with resected pGGNs also had no cases of recurrence at five years in comparison to a 6.3 recurrence rate in study participants with heterogeneous GGNs and a 10.8 percent recurrence rate for patients with PSNs, according to the study authors.
“In the present study, when requiring subsolid nodules to be truly homogeneous to be classified as pGGNs, no resected pGGN developed subsequent locoregional or distant recurrence, supporting an indolent course for these lesions. Therefore, we believe that imaging surveillance is a reasonable management plan for strictly defined pGGNs,” wrote study co-author Mark M. Hammer, M.D., who is an assistant professor at Harvard Medical School and program director of the cardiothoracic imaging fellowship at Brigham and Women’s Hospital in Boston, and colleagues.
Three Key Takeaways
- Low recurrence rates in resected pGGNs. The study highlights that patients with resected pure ground-glass nodules (pGGNs) exhibit very low recurrence rates up to seven years after treatment. This suggests that pGGNs may have an indolent course, supporting the idea that imaging surveillance is a reasonable management plan for strictly defined pGGNs.
- Differences in invasive adenocarcinoma frequency. Patients with resected pGGNs had a significantly lower frequency of invasive adenocarcinoma (39 percent) compared to patients with heterogeneous GGNs (67.9 percent) and part-solid nodules (PSNs) (75.7 percent). This implies that pGGNs may represent a distinct subgroup of subsolid nodules with less aggressive behavior.
- Improved long-term survival in patients with pGGNs. The study reports that seven years after resection, patients with pGGNs demonstrated higher recurrence-free survival (97.7 percent) and overall survival rates (97.7 percent) compared to those with heterogeneous GGNs (recurrence-free survival: 82 percent, overall survival: 84.6 percent) and PSNs (recurrence-free survival: 79.4 percent, overall survival: 82 percent). These findings suggest that pGGNs may have a more favorable prognosis than other subsolid nodules.
Seven years after resection, the researchers found that 97.7 percent of patients with pGGNs had recurrence-free survival (RFS) in comparison to 82 percent of study participants with heterogeneous GGNs and 79.4 percent of those with PSNs. The study authors also noted significant differences in seven-year overall survival rates for patients with pGGNs (97.7 percent) in contrast to those with heterogenous GGNs (84.6 percent) and PSNs (82 percent).
“The findings suggest that pGGNs and heterogeneous GGNs may represent distinct subgroups of subsolid nodules with respect to aggressiveness and prognosis,” noted Hammer and colleagues.
(Editor’s note: For related content, see “Nine Takeaways from Recent Meta-Analysis on Lung Cancer Screening with Low-Dose CT,” “COVID-19 and Cancer: What a New Chest CT Study Reveals” and “How Socioeconomic Disparities Affect Follow-Up of Incidental Pulmonary Nodules on CT.”)
Beyond the inherent limitations of a single-center retrospective study, the authors noted heterogeneous follow-up duration as well as varied CT protocols with respect to contrast media use and slice thickness. The researchers also acknowledged the study cohort was limited to patients who had surgical resection of confirmed adenocarcinoma.