An emerging deep learning model for predicting future fracture risk in patients with hip fractures — based upon digitally reconstructed X-rays from three-dimensional computed tomography (3D CT) hip scans — demonstrated higher area under the curves (AUCs) for two-, three- and five-year risk projections than multiple clinical models based on known risk factors.
For the retrospective study, recently published in Radiology, researchers reviewed data from 1,480 patients (mean age of 75.5) with a hip fracture who had a hip CT scan. Utilizing a training and validation dataset of 1,012 patients and a temporal test set comprised of 468 patients, the researchers compared the prognostic capacity of the aforementioned deep learning model to multiple imaging and clinical models.
In comparison to hip radiography in the test set, the study authors found that that the 2.5-dimensional ensemble model had a 12 percent higher concordance index (C-index) (73 percent vs. 61 percent), a nine percent higher three-year AUC (74 percent vs. 65 percent) and a 16 percent higher five-year AUC (73 percent vs. 57 percent) for predicting future fracture risk.
The deep learning model also demonstrated a higher C-index, two-year AUC (74 percent), three-year AUC and five-year AUCs than scout film from CT, frontal, axial and lateral digitally reconstructed radiographs (DRRs) and a 3D volume imaging model, according to test set data from the study.
The study authors also noted that 2.5-dimensional ensemble model outperformed the two- and three-year AUCs for multiple clinical models. They pointed out a 16 percent higher two-year AUC (74 percent) and a 10 percent higher three-year AUC (74 percent) for the deep learning model in comparison to a clinical model (58 percent and 64 percent respectively) that assessed 10 known clinical risk factors for fractures, including femoral neck BMD and hip fracture type.
“Developing a prediction model for short-term subsequent fracture risk is important because it would identify patients at the highest risk and aid in determining appropriate treatment strategies,” wrote lead study author Yisak Kim, M.S., who is affiliated with the Interdisciplinary Program in Bioengineering at the Seoul National University Graduate School and the Department of Radiology at the Seoul National University Hospital in Seoul, Korea, and colleagues.
Three Key Takeaways
- Improved predictive performance. The deep learning model, based on digitally reconstructed X-rays from 3D CT hip scans, outperformed multiple clinical models in predicting future fracture risk for hip fracture patients.
- Enhanced imaging model performance. When compared to traditional hip radiography, the 2.5-dimensional ensemble deep learning model consistently showed higher concordance index (C-index) and AUCs. Specifically, it exhibited a 12% higher C-index, a 9% higher three-year AUC, and a significant 16% higher five-year AUC for predicting future fracture risk. The deep learning model also outperformed scout film from CT, frontal, axial, and lateral digitally reconstructed radiographs (DRRs), and a 3D volume imaging model for predicting future fracture risk in hip fracture patients.
- Short-term subsequent fracture risk prediction. The deep learning model surpassed clinical models in predicting short-term subsequent fracture risk. In comparison to one clinical model that assessed 10 known risk factors, including femoral neck BMD and hip fracture type, the deep learning model demonstrated a 16% higher two-year AUC and a 10% higher three-year AUC, underscoring its potential in identifying patients at the highest risk and aiding in determining appropriate treatment strategies for patients with hip fractures.
Emphasizing that this is the first study to develop a prediction model for future fracture risk in hip fracture patients, the study authors noted that utilizing hip CT as a basis for the deep learning model was particularly beneficial.
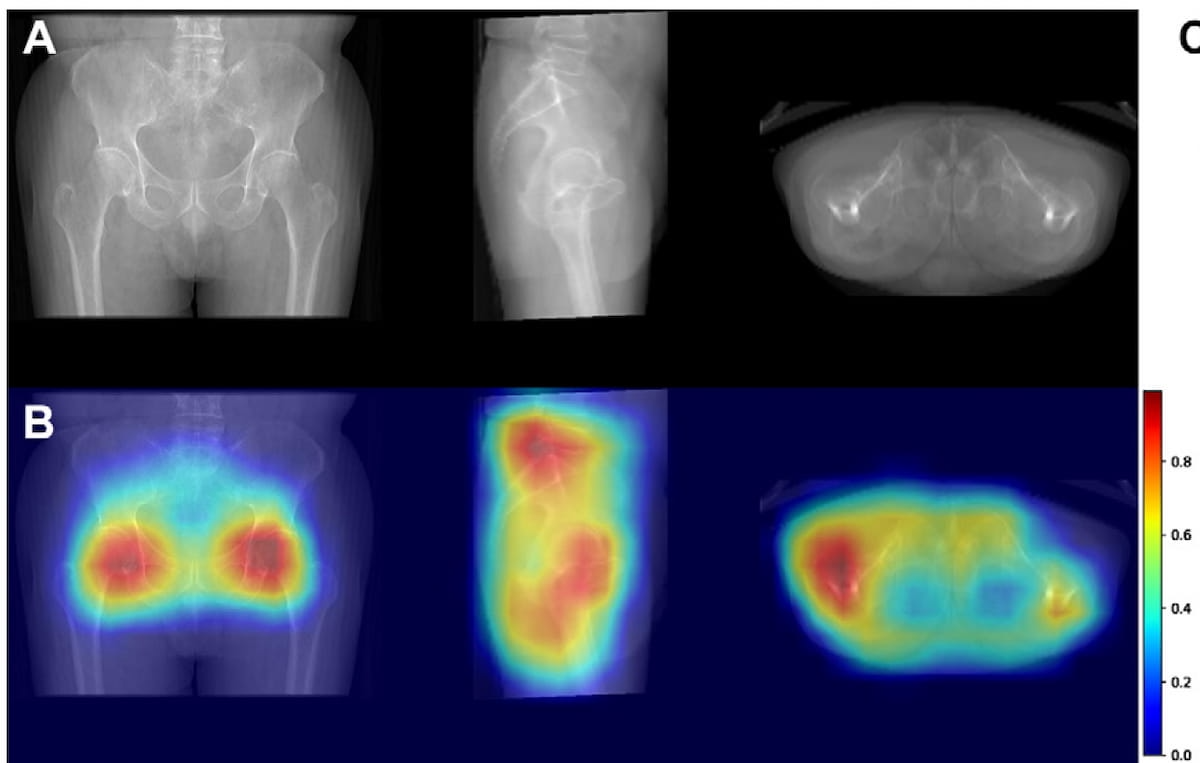
“ … A model using images of various hip CT angles performed better compared with models with front cross-sectional images, such as anteroposterior radiographs, suggesting the potential use of the 2.5-dimensional model with other CT images,” noted Kim and colleagues.
(Editor’s note: For related content, see “AI Facilitates Nearly 83 Percent Improvement in Turnaround Time for Fracture X-Rays,” “OsteoSight Gets FDA Breakthrough Device Designation for Bone Mineral Density Assessment on X-Rays” and “Gleamer’s BoneView Gains FDA Clearance for AI-Powered Pediatric Fracture Detection.”)
In regard to study limitations, the authors noted the use of 3D hip CT may limit broader extrapolation of the study findings. While heat maps with the deep learning model primarily highlighted femur neck and shaft areas, the researchers conceded a widely varied focus area among patients in the cohort. They also acknowledged that excluding denosumab users from the training and validation set may have affected the performance of the deep learning model.