Diagnostic Imaging Europe
- Diagnostic Imaging Europe Vol 26 No 7
- Volume 26
- Issue 7
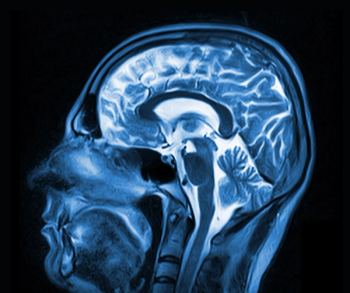
3T MR shows cardiac scarring and vasculature
Experts have long suggested that the clinical promise of 3T, with its improved signal-to-noise ratio compared with 1.5T, might eventually be expressed in cardiac imaging, one of the least approachable clinical areas of MR.
Experts have long suggested that the clinical promise of 3T, with its improved signal-to-noise ratio compared with 1.5T, might eventually be expressed in cardiac imaging, one of the least approachable clinical areas of MR. A new imaging technique developed at the University of Western Ontario is fueling that optimism with high-resolution 3D images of cardiac vasculature and scar tissue in the heart muscle.
“This is the first time we have been able to visualize myocardial (scarring) and the heart’s blood vessels at the same time,” said Dr. James White, an assistant professor of medicine at the university.
The resulting 3D model of the heart allows interpreters to immediately understand the relationship between the heart’s blood vessels and related permanent injury, he said.
White and colleagues begin by continuously infusing gadolinium-based contrast, creating a high-resolution, volumetric image of the heart showing coronary blood vessels. The contrast medium remains longer in scar tissue than in healthy muscle or the vasculature. A repeat scan, performed 20 minutes later, highlights the scarring because the two data sets, which are taken using the exact same pulse sequence, are fused into a 3D model.
White and colleagues at the University of Western Ontario Robarts Research Institute reported results using this technique on 55 patients in the September online Journal of the American College of Cardiology: Cardiovascular Imaging. Patients were referred to the research team for either bypass surgery or cardiac resynchronization therapy (CRT), which involves implantation of a specialized pacemaker designed to improve heart function. The MR studies were performed to demonstrate whether the proposed procedures were likely to have the intended result, and, in the process, whether the MR technique could be valuable in the planning of these vascular-based cardiac interventions.
In bypass or angioplasty procedures, surgeons must decide whether to open blocked blood vessels. If scar tissue is seen in the region, no benefit will be expected. Similarly, scar tissue in muscle where CRT leads are placed might prevent patients from benefitting from the pacemaker.
White and colleagues conclude that their MR-based 3D cardiac model helps surgeons and cardiologists better understand the cardiac status of the patient.
“We’ve known for some time that myocardial scar tissue can be imaged using MRI, but what we’ve now been able to do is to take this imaging to another level,” he said. “This (3D model) will help direct surgeons and cardiologists to better target the blood vessels that lead to muscle capable of responding to their therapy, rather than to muscle that is irreversibly diseased.”
Articles in this issue
over 15 years ago
Radiologists question whether to treat small pulmonary emboliover 15 years ago
Overlap shifts help urgent findings communicationover 15 years ago
Delayed cardiac test saves moneyover 15 years ago
Incidental findings can predict cardiac diseaseover 15 years ago
MRI reveals when cognitive impairment will advanceover 15 years ago
Broad view of heart shows otherwise missed diagnosesover 15 years ago
Spectral CT beats CT at illuminating heart plaqueover 15 years ago
California gets landmark dose reporting lawover 15 years ago
Radiation increases risk of leukemia for interventionalistsover 15 years ago
Readers' diagnostic accuracy drops as the day goes onNewsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.