Intraprocedural CT reduces recurrent kidney tumors
Intraprocedural contrast-enhanced CT reduces the rate of incompletely treated renal cell carcinoma by nearly 64%, according to a study presented at the jointly-sponsored RSNA/SIR Foundation Interventional Oncology Symposium.
Intraprocedural contrast-enhanced CT reduces the rate of incompletely treated renal cell carcinoma by nearly 64%, according to a study presented at the jointly-sponsored RSNA/SIR Foundation Interventional Oncology Symposium.
In addition, the study found that larger tumors are more likely to recur, suggesting that such intraprocedural imaging may be particularly useful in treating larger lesions.
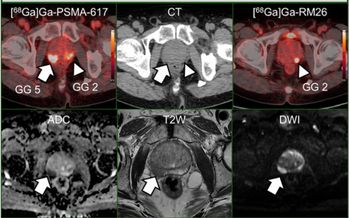
Contrast-enhanced CT reveals residual tumor during treatment with radiofrequency ablation. Remaining malignant tissue was immediately ablated, and there was no recurrence at three-month follow-up. (Provided by K. Krehbiel)
The retrospective study of 90 tumors in 82 patients with stage I and II renal cell carcinoma divided patients into two groups based on creatinine level. Patients with creatinine levels of 2.0 or less underwent a CECT study after the tumor was presumed fully ablated. Patients with a creatinine level higher than 2.0 were not scanned, and the ablation endpoint was determined by the estimated ablation zone.
Intraprocedural CECT found residual tumors in 10% of patients, said Dr. Kyle A. Krehbiel of Wake Forest University in North Carolina. The team used CECT to target the residual tumor and immediately re-ablated the area.
After an average follow-up of 10 months, the team discovered recurrent disease in 5.8% of patients who underwent intraprocedural CECT. By contrast, 19% of patients who did not receive intraprocedural CECT experienced recurrent disease.
On follow-up, the team discovered none of the residual tumors that had required additional ablation recurred. However, 6.4% of tumors showed no enhancement with CECT recurrent disease on follow-up imaging, indicating that the CECT may miss microscopic viable tumor cells.
The size of the lesion seemed to influence the rate of recurrent disease. The average size of lesions in either group that showed residual or recurrent tumor was 4.3 cm, while lesions that did not show residual or recurrent tumor were 2.5 cm on average.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.