Is Digital Breast Tomosynthesis Superior to Digital Mammography?
A closer look at the literature suggests the combination of digital breast tomosynthesis (DBT) and two-dimensional (2D) digital mammography (DM) has relatively equivalent cancer detection rates as using DM alone, according to a recent presentation at the Society of Breast Imaging (SBI)/American College of Radiology (ACR) conference.
Has digital breast tomosynthesis (DBT) lived up to the initial hype when it comes to breast cancer detection?
In her recent lecture on DBT at the Society of Breast Imaging (SBI)/American College of Radiology (ACR) conference, Debra Monticciolo, MD, FACR, FSBI, said DBT and two-dimensional (2D) digital mammography (DM) “are closer cousins than we expected.”
In five European studies comparing DM/DBT to DM that were published prior to 2018, the cancer detection rate (CDR) was incrementally better than that of DM, but Dr. Monticciolo said there are key caveats to consider with these studies. These studies emphasized biennial screening, which increases CDR and most of these studies had an older population (over 50 years of age) with a higher underlying prevalence of disease, which increases CDR, pointed out Dr. Monticciolo, the Dr. Robert and Alma Moreton Centennial Chair in Radiology and a professor of radiology and vice-chair for research with Baylor Scott and White Health, Texas A&M University.
Dr. Monticciolo said the American retrospective studies (emphasizing annual screening) prior to 2018 showed variable results in comparing CDRs between DBT and DM. Of the subsequent retrospective American studies published in 2018 and beyond comparing DM/DBT and DM, “there is no statistically significant difference in many of the studies for CDR,” noted Dr. Monticciolo, a past president of the American College of Radiology and the Society of Breast Imaging.
There is also conflicting data when it comes to comparing recall rates between DM/DBT and DM, according to Dr. Monticciolo. She noted that DM/DBT had a 4.14 average recall rate in five European studies published prior to 2018 and DM had a 3.58 average recall rate. Yet in U.S. retrospective studies prior to 2018, the average recall rate was 8.0 for DM/DBT and 11.3 for DM. However, in seven recent studies published in 2018 and beyond, Dr. Monticciolo pointed to improved recall rates with DBT, noting average recall rates of 7.72 for DBT and 9.0 for DM.
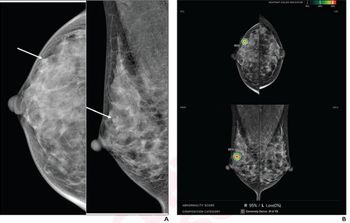
In her SBI/ACR lecture, Dr. Monticciolo also looked at the viability of synthesized mammography (SM) in possibly replacing the use of DM in DM/DBT. While the use of SM reduces image acquisition and the combination of SM/DBT reportedly reduces radiation dose by approximately 40 percent in comparison to DM/DBT, Dr. Monticciolo said there has a been a slow adoption of SM among radiologists since the availability of the technology in 2013. She noted one 2017 study of over 1,150 breast radiologists found that approximately 75 percent had SM but utilized DM/DBT.
This boils down to inferior spatial resolution for SM, according to Dr. Monticciolo, the section chief of breast imaging at Baylor Scott and White Healthcare, Texas A&M University. She said SM accentuates high contrast objects, but problems arise at points close to resolution threshold.
“There isn’t a breast imager anywhere who would rather read (a SM image) than a standard DM view,” maintained Dr. Monticciolo. “ … There is no question that SM is an inferior image.”
She noted that a 2021 meta-analysis compared SM/DBT versus DM and DM.DBT. In 11 studies that compared SM/DBT and DM, the use of SM/DBT resulted in a higher CDR.Yet in seven studies that compared SM/DBT with DM/DBT, there was no difference in CDR, according to Dr. Monticciolo. She noted the authors of the meta-analysis found that SM/DBT screening offered similar detection rates for all cancer, invasive cancer, and ductal carcinoma in situ (DCIS) in comparison to DM/DBT as well as a lower biopsy rate and recall rate.
Dr. Monticciolo said three other meta-analyses published in 2021 found equivalent CDR between SM/DBT and DM/DBT.
She added that the recently published STORM-2 trial found that SM/DBT and DM/DBT were equivalent in regard to CDR, and both had a higher CDR than DM. However, while these findings held up for patients 60 years of age and younger, “the (CDR) advantage of SM/DBT disappears and the advantage of DM/DBT narrows” for patients over the age of 60,” noted Dr. Monticciolo.
“If you’re doing SM/DBT, you can feel good because the outcomes are probably going to be equivalent with DM/DBT,” summarized Dr. Monticciolo. “If you’re using DM/DBT, you can feel good because you are giving your patient the highest resolution exam that you can and as long as you stay within the federal (radiation) exposure limits, it’s completely safe.”
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.














