Mammography Study Suggests DBT-Based AI May Help Reduce Disparities with Breast Cancer Screening
New research suggests that AI-powered assessment of digital breast tomosynthesis (DBT) for short-term breast cancer risk may help address racial disparities with detection and shortcomings of traditional mammography in women with dense breasts.
Can artificial intelligence (AI) play a role in mitigating disparities with breast cancer screening?
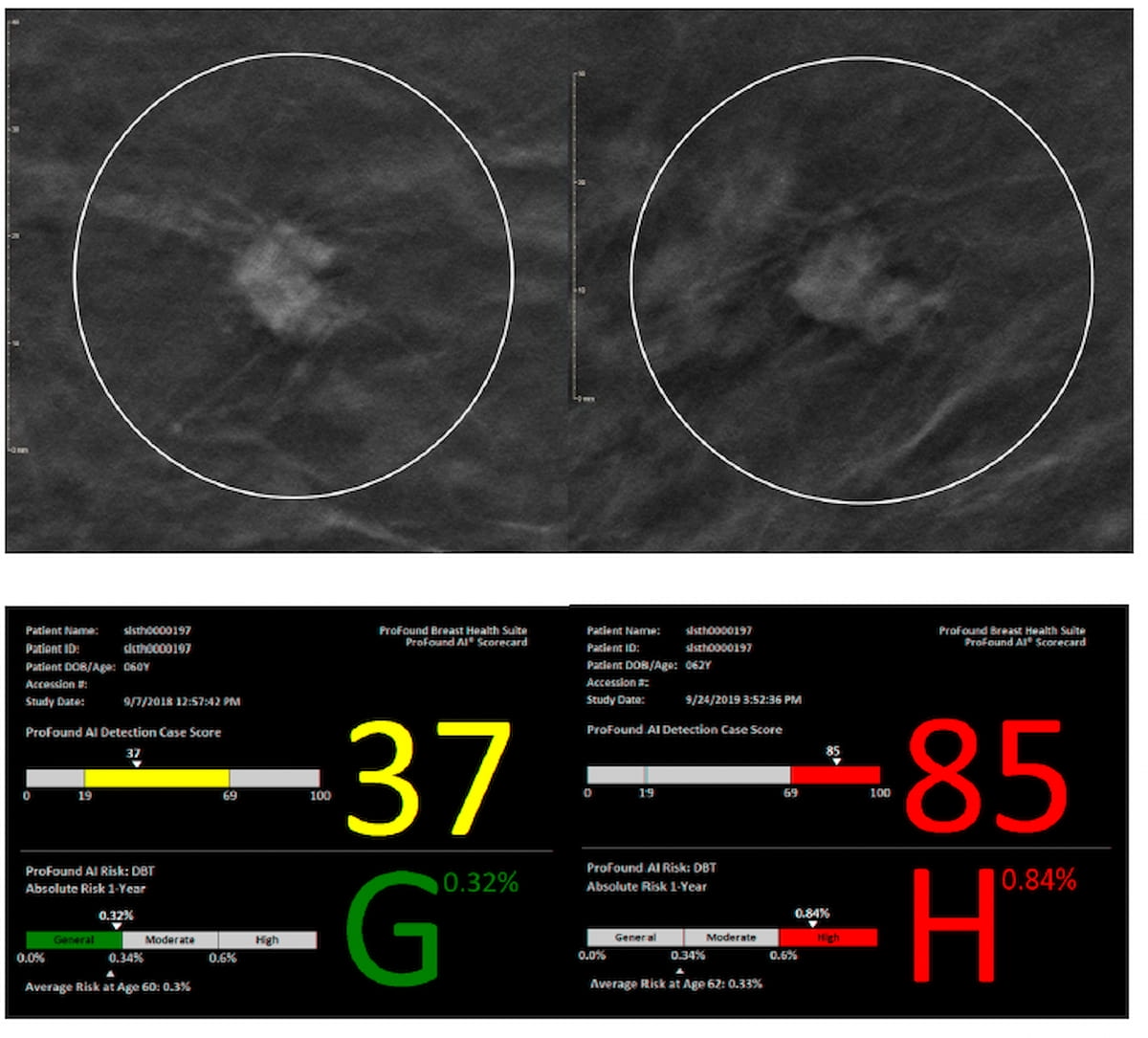
For the multicenter study, presented at the 2024 San Antonio Breast Cancer Symposium (SABCS), researchers evaluated the ProFound AI Breast Health Suite (iCAD) for assessing short-term breast cancer risk based on digital breast tomosynthesis (DBT) images for 3,558 women. The cohort included 394 cases of breast cancer detection, according to the study. For the ProFound AI Breast Health Suite, one-year AI risk scores < 34 percent denote average risk, scores between 34 percent and 60 percent reveal intermediate risk and scores > 60 percent are considered high-risk scores.
Here one can see a non-spiculated mass on the upper left mammography image for a 62-year-old Black woman who had scattered fibroglandular densities at initial screening and a grade 3 invasive ductal carcinoma detect in subsequent mammography screening (upper right) with the AI detection score (below) increasing from 37 to 85. (Images courtesy of 2024 San Antonio Breast Cancer Symposium (SABCS) and iCad.)
Overall, women with intermediate risk scores comprised 13.1 percent of the cohort, high-risk scores accounted for 18.2 percent of the study participants and the remaining 68.7 percent of the cohort had average risk scores.
While acknowledging differences in the racial composition of the adjusted high-risk screening population, the study authors noted similarities in breast cancer prevalence for those who had high AI one-year risk scores. In this group, the researchers pointed out a 1 in 38 prevalence of breast cancer in White women, a 1 in 41 prevalence in Black women, a 1 in 34 prevalence for Asian women and a 1 in 55 prevalence for women of other races.
“The case scores did not vary significantly across racial subgroups in our dataset, suggesting that the accuracy of the AI software was consistent across races,” noted Chirag Parghi, M.D., M.B.A., the chief medical officer for Solis Mammography.
The study authors also noted similarities in AI high-risk scoring between women with dense breasts and those with non-dense breasts. For women with dense breasts and high AI risk scores, the breast cancer prevalence was 1 in 36 in comparison to a 1 in 41 prevalence for women with non-dense breasts and high AI risk scores, according to the researchers.
“Based on our results, image-based risk can potentially offset known gaps in breast cancer detection by traditional mammography in patients with dense tissue and address known disparities across races,” emphasized Parghi and colleagues.
Reference
1. Parghi C, Pantleo J, Shisler J, et al. Image-derived short term breast cancer risk score in the analysis of breast cancer prevalence in screening population by race and breast density. Poster presented at the 2024 San Antonio Breast Cancer Symposium (SABCS) December 10-13, San Antonio, Texas.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.
Considering Breast- and Lesion-Level Assessments with Mammography AI: What New Research Reveals
June 27th 2025While there was a decline of AUC for mammography AI software from breast-level assessments to lesion-level evaluation, the authors of a new study, involving 1,200 women, found that AI offered over a seven percent higher AUC for lesion-level interpretation in comparison to unassisted expert readers.
FDA Clears Virtually Helium-Free 1.5T MRI System from Siemens Healthineers
June 26th 2025Offering a cost- and resource-saving DryCool magnet technology, the Magnetom Flow.Ace MRI system reportedly requires 0.7 liters of liquid helium for cooling over the lifetime of the device in contrast to over 1,000 liters commonly utilized with conventional MRI platforms.