Qualitative Radiology Reports Insufficient for Tumor Burden
PACS would enhance and promote collaboration between radiologists and oncologists and improve quantitative reporting of tumors.
Quantitative interactive reporting is better than traditional text-only qualitative reporting for assessing tumor burden in cancer trials, according to a study published in the
Researchers from the United States and Israel sought to determine what oncologists and radiologists thought about quantitative interactive and multimedia reporting in relation to clinical efficacy and response to established and evolving therapeutic agents in cancer trials.
Twenty-eight of 35 radiologists and 109 of 253 oncologists (who treated more than 40 tumor types) and registrars from the researchers’ facility responded to a questionnaire about current reporting methods, methods for Response Evaluation Criteria in Solid Tumors (RECIST) tumor measurement, and preferred reporting format.
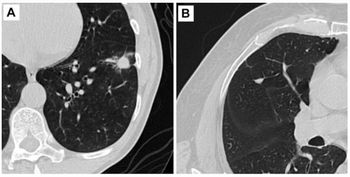
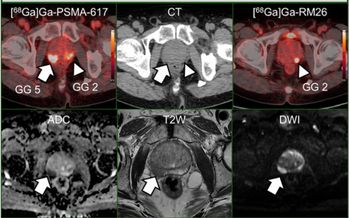
According to the findings, 67 of the oncologists (65.7%) and 12 radiologists (44.4%) felt that the current traditional qualitative radiology reports were insufficient for reporting tumor burden and communicating measurements. Twenty-one of the radiologists (77.8%) and 71 oncologists (85.5%) agreed that key images with measurement annotations helped in finding previously measured tumors; however, only 43% of radiologis[[{"type":"media","view_mode":"media_crop","fid":"42617","attributes":{"alt":"","class":"media-image media-image-right","id":"media_crop_1499751251467","media_crop_h":"0","media_crop_image_style":"-1","media_crop_instance":"4633","media_crop_rotate":"0","media_crop_scale_h":"0","media_crop_scale_w":"0","media_crop_w":"0","media_crop_x":"0","media_crop_y":"0","style":"height: 133px; width: 199px; border-width: 0px; border-style: solid; margin: 1px; float: right;","title":"©Kamira/Shutterstock.com","typeof":"foaf:Image"}}]]ts regularly saved key images, said the authors.
The physicians were also asked their opinions regarding hyperlinking measurements from the reports to images of the lesions; 70 of the oncologists (64.2%) and 19 of the radiologists (67.9%) preferred this approach over text-only reports. “Approximately 60 percent of oncologists indicated that they handwrote tumor measurements on RECIST forms, and 40 percent used various digital formats,” the authors wrote. “Most of the oncologists (93 percent) indicated that managing tumor measurements within a PACS would be superior to handwritten data entry and retyping of data into a cancer database.”
The researchers concluded that a PACS reporting system that enhanced and promoted collaboration between radiologists and oncologists would improve quantitative reporting of tumors.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.