SNMMI: AI May Enhance Detection and Risk Assessment for Multiple Cancers on Whole-Body PET/CT Scans
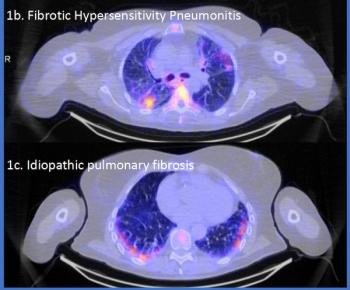
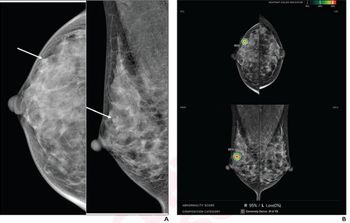
Deep transfer learning may elevate the capability of whole-body PET/CT scans to diagnose multiple cancers, ranging from breast cancer and lung cancer to melanoma and prostate cancer, according to new research presented at the SNMMI conference.
The use of artificial intelligence (AI)-powered tumor segmentation on whole-body positron emission tomography/computed tomography (PET/CT) scans yielded median true positive rates (TPRs) of 75 percent, 85 percent, 87 percent, and 75 percent, respectively, for lung cancer, melanoma, lymphoma, and prostate cancer, according to research presented at the
For the study, researchers developed a deep transfer learning model in order to facilitate automated tumor segmentation on whole-body PET/CT scans. The model was trained on 611 FDG PET/CT scans from patients with a variety of lung cancers including head and neck cancer, lymphoma, lung cancer, breast cancer and melanoma, according to the study. The study authors noted the model training also included 408 PET/CT scans from patients with prostate cancer.
“Most AI models that aim to detect cancer are built on small to moderately sized datasets that usually encompass a single malignancy and/or radiotracer,” noted Kevin H. Leung, M.D., a research associate at Johns Hopkins University School of Medicine. “This represents a critical bottleneck in the current training and evaluation paradigm for AI applications in medical imaging and radiology.”
In addition to the aforementioned TPR data, the researchers noted that the deep transfer learning model had median positive predictive values (PPVs) of 92 percent for lung cancer, 76 percent for melanoma, 87 percent for lymphoma, and 76 percent for prostate cancer.
The deep transfer learning model also predicted prostate cancer with an 83 percent accuracy rate and an 86 percent area under the receiver operating characteristic curve (AUROC), according to the researchers. They pointed out that the model’s classification of these patients with low, intermediate, and high risk correlated with mean follow-up prostate-specific antigen (PSA) levels of 9.18, 26.92 and 727.46 ng/ml respectively.
“In addition to performing cancer prognosis, the (deep transfer learning) approach provides a framework that will help improve patient outcomes and survival by identifying robust predictive biomarkers, characterizing tumor subtypes, and enabling the early detection and treatment of cancer,” emphasized Leung. “The approach may also assist in the early management of patients with advanced, end-stage disease by identifying appropriate treatment regimens and predicting response to therapies, such as radiopharmaceutical therapy.”
Reference
1. Leung K, Rowe SP, Sadaghiani MS, et al. Fully automated whole-body tumor segmentation on PET/CT using deep transfer learning. Presented at the 2024 Society of Nuclear Medicine and Molecular Imaging Annual Meeting, June 8-11, Toronto, Canada. Available at:
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.