
While this author has no intention of retiring from radiology, he notes that retiring from certain work schedules or aspects of the field have had a favorable impact on his life.

Eric Postal, MD, is a diagnostic radiologist with the University of Pittsburgh Medical Center.

While this author has no intention of retiring from radiology, he notes that retiring from certain work schedules or aspects of the field have had a favorable impact on his life.

While there may be awkwardness and a degree of embarrassment in noting obvious findings to referring clinicians in radiology, consistent communication of those findings is essential.

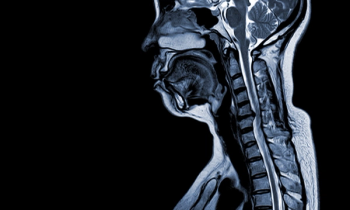
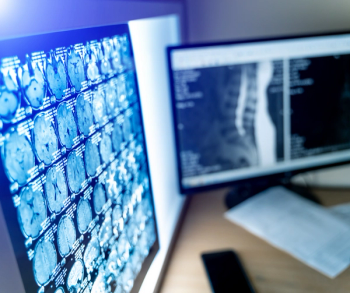
How strong is your own quality assurance (QA) barometer for interpreting CT, MRI, and ultrasound images?

I’ve long since learned that good faith is far more reliable than, say, contracts.

When facilities routinely forward X-rays for “pain,” vascular ultrasound studies without Doppler or chest computed tomography (CT) scans devoid of breath holding, patient care suffers.
When you are asked for an informal medical opinion, one’s intellectual curiosity and desire to help others never fade away.

Does access to prior imaging results have to be mission impossible for teleradiologists?
What do you do with a CD of imaging that has no information on the doc requesting the radiologist read?

Addressing ancillary repetitious inhibitors to radiology workflow could go a long way to mitigating burnout risk.

The notion of non-physician practitioners (NPPs) attempting to do radiologist-level work is a very slippery slope and what this author refers to as the “bargaining” stage of grief.

Superfluous pan scans have become standard for a vast majority of minor injury presentations in emergency room settings.

While it stands to reason that referring physicians would prefer a condensed summary of relevant imaging findings, vagaries with insurers, patients and other possible readers of the radiology report may warrant an inefficient minutiae-cluttered approach.

There are cases that warrant verbal communication with referring clinicians, but making that communication happen can, at times, be a challenging responsibility.

While some may equate extra work hours as honorable self-sacrifice or dedication to patients, striving for an optimal balance of life and work is an individual choice that shouldn’t be criticized.
When reviewing radiographs, computed tomography (CT) scans or magnetic resonance imaging (MRI) scans, do you still turn to mnemonics every now and then to jog your short-term memory?

Whether it’s attempting to get appropriate clinical histories from referring physicians or getting a tech to split up a multiphasic contrast study into separate image series, consistently striving to fight the good fight for optimal image interpretation is worth the effort.

Whether it’s the proverbial “bad penny” case that crashes PACS or the perception that positive computed tomography angiography (CTA) exams for pulmonary arterial clots come in sets of three, suspicions can emerge here and there in radiology.

This author emphasizes that diplomacy is always the best policy when leaving one radiology employer for another.

This author emphasizes keys to being engaging and informative during a lecture.

One of the hallmarks of career savvy is recognizing when changes in worklist demands or compensation require adapting as a team player or adapting to a new change of scenery.

Lamenting a lack of control over imaging requests from referring clinicians, this author suggests that a more collaborative approach between referrers and radiologists may facilitate more efficient use of imaging.

Has a form of aversive conditioning sabotaged morale in radiology?

A continued emphasis on sharpening skills, robust networking and living within one’s means are keys to navigating the ups and downs of the radiology job market.

Is there a certain line of self-preservation in radiology reporting for findings and impressions?

A good awareness of your communication style with others can pay significant dividends in your career.

While social media posts abound about the impact of the residency match in different fields and other topics, this author encourages perspective that is grounded in the facts.
In an age of robust imaging volume, time constraints and challenges with voice recognition software, attention to detail with verbiage in radiology reports may suffer.

In addition to the advantages of working remotely, this author says teleradiology increases competition, collaboration and growth for radiologists and rad groups alike.

From pagers, transcriptionists, and low-tech X-rays to teleradiology, advanced imaging and artificial intelligence (AI), this author considers the evolution of radiology over three decades.

Can more easygoing radiologists coexist with productivity-driven colleagues?