
Catch up on the top radiology content of the past week.
An update to Quantib Prostate 2.1, Quantib Prostate 3.0 reportedly facilitates workflow advances and offers a variety of tools, ranging from artificial intelligence (AI)-based segmentation to PI-RADS scoring support, to help improve interpretation of prostate magnetic resonance imaging (MRI).

Catch up on the top radiology content of the past week.
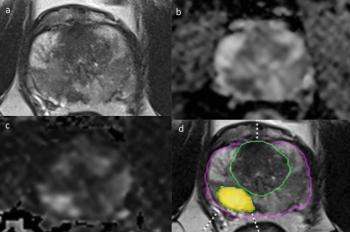
In a recent study of a deep learning software in patients with suspected prostate cancer, researchers noted no difference in the detection of clinically significant prostate cancer nor PI-RADS scoring consistency.
The expanded indication could facilitate improved access to imaging for patients with metastatic prostate cancer who are candidates for radioligand treatment.

In a video interview from the recent American Society of Clinical Oncology Genitourinary Cancers (ASCO GU) Symposium, Brian Chapin, MD, discussed emerging research that demonstrated the ability of the positron emission tomography (PET) agent 18F-rhPSMA-7.3 to diagnose distant M1 lesions prior to surgery for patients with intermediate to high-risk prostate cancer.
New research from the American Cancer Society comparing pre-pandemic cancer screening prevalence to the second year of the COVID-19 pandemic in the United States showed a 1.1 million decrease in breast cancer screenings, a 4.4 million decrease in cervical cancer screening and a 600,000 decrease in prostate cancer screenings.

Catch up on the top radiology content of the past week.

Use of the prostate-specific membrane antigen (PSMA) positron emission tomography (PET) agent piflufolastat F 18 led to treatment plan changes in nearly 40 percent of men with recurrent prostate cancer and low prostate-specific antigen (PSA) levels, according to new research presented recently at the 2023 American Society of Clinical Oncology (ASCO) Genitourinary Cancers (GU) Symposium in San Francisco.

Catch up on the top radiology content of the past week.

In a recent video interview, Amar Kishan, M.D., discussed a new study that demonstrated significant side effect reduction when utilizing magnetic resonance imaging (MRI) guidance instead of computed tomography (CT) guidance for stereotactic body radiation therapy (SBRT) to treat localized prostate cancer.

A new study found that approximately one-third of men with prostate cancer were diagnosed with at least one vertebral fracture prior to the initiation of androgen deprivation therapy (ADT).

Check out the top radiology content of the past week.
A new comparative study found the use of prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) led to treatment changes in nearly 20 percent of patients with high-risk prostate cancer.
Catch up on the top AI-related news and research of the past month.

Check out the top radiology content of the past week.
In a study of nearly 18,000 men who had prostate cancer screening, researchers found the use of pre-biopsy magnetic resonance imaging (MRI) for those with elevated prostate-specific antigen (PSA) levels and reserving MRI-targeted biopsy for those with PI-RADS scores of 3 to 5 reduced the risk of detecting clinically insignificant cancers by half.

Catch up on the top radiology content of the past week.
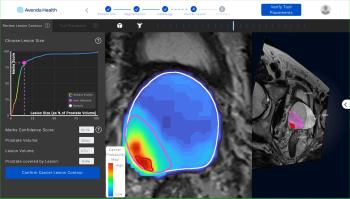
The Food and Drug Administration has granted 510(k) clearance to iQuest (Avenda Health), an artificial intelligence (AI) platform that combines findings from magnetic resonance imaging (MRI), pathology reports and biopsy results to facilitate three-dimensional mapping of prostate cancer.
For patients recently diagnosed with prostate cancer, the emerging positron emission tomography (PET) agent 18F-rhPSMA-7.3 reportedly has a 96 percent specificity rate for detecting pelvic lymph node metastases, according to Phase 3 study results recently presented at the 22nd Annual Scientific Meeting of the Society of Urologic Oncology (SUO).

Catch up on the top radiology content of the past week.
In what may be the first study to assess the effectiveness of biparametric magnetic resonance imaging (MRI) for prostate cancer screening in a large cohort, researchers found that MRI screening had a significantly lower false positive rate and significantly higher positive predictive values (PPVs) than prostate-specific antigen (PSA)-based screening.
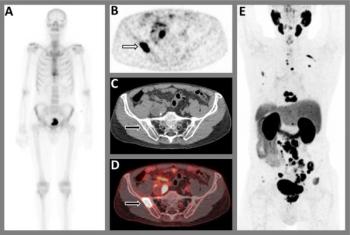
New research shows that 18F-NaF PET/CT had higher sensitivity, accuracy, and negative predictive value than 99mTc-MDP SPECT for bone metastases in patients deemed to be at high risk for prostate cancer or breast cancer.

Catch up on the top radiology content of the past week.
For patients undergoing stereotactic body radiotherapy (SBRT) for prostate cancer, the acute genitourinary (GU) toxicity rate associated with the procedure was 19 percent lower with magnetic resonance imaging (MRI) guidance in comparison to computed tomography (CT) guidance, according to new research presented recently at the American Society for Radiation Oncology (ASTRO) Annual Meeting.

In a recent video interview from the American Society for Radiation Oncology (ASTRO) Annual Meeting, Benjamin Lowentritt, MD discussed the challenges of conventional imaging in diagnosing prostate cancer recurrence and the potential of an emerging high affinity, radiohybrid prostate-specific membrane antigen/positron emission tomography (PSMA/PET) imaging agent.
Five weeks of radiation therapy is just as effective as eight weeks of radiation treatment for men with high-risk prostate cancer, according to new research presented at the American Society for Radiation Oncology (ASTRO) Annual Meeting.