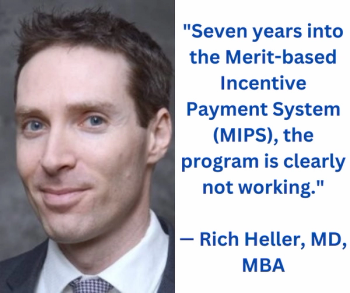
Noting that the Medicare conversion factor in 2024 could be lower than the rate in 1993, this author discusses three key issues that need to be addressed by government leaders in order to ensure equitable Medicare reimbursement for radiologists and other physicians.