Multiple factors influence breast ultrasound performance
Preliminary findings from a national trial of ultrasound as a screening tool in patients at high risk for breast cancer shed light on key variables that influence radiologist interpretive performance.
Preliminary findings from a national trial of ultrasound as a screening tool in patients at high risk for breast cancer shed light on key variables that influence radiologist interpretive performance.
In the first of two studies based on the American College of Radiology Imaging Network 6666 trial and presented at the RSNA meeting on Monday, investigators assessed the impact on interpretive performance of several factors. The factors ranged from breast imaging experience to personal participation in patient scanning.
After a one-hour didactic session on BI-RADS ultrasound categories, 35 radiologists with at least two years of experience in breast imaging reviewed 70 proven cases. The physicians interpreted the cases twice: initially without feedback, and again with immediate feedback based on pathology findings.
Regardless of all other variables, performance improved across the board after feedback, said Dr. Wendie Berg, chief investigator of the ACRIN trial, which is supported by the Avon Foundation and the National Cancer Institute.
But some radiologists performed markedly better than others. The top docs included those who spend at least 25% of their time interpreting breast imaging studies, personally participate in patient scanning, or perform at least 20 to 40 ultrasound exams weekly.
Although radiologists with more experience performed better than those with less, that particular advantage peaks at six to 10 years in breast imaging, Berg said. Performance scores declined in radiologists with 10 or more years of experience.
The lowest performance scores came from radiologists who work at sites where technologists scan patients without any physician involvement.
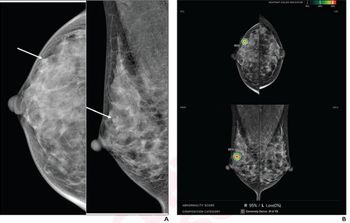
In a second study based on the ACRIN trial, Berg evaluated radiologists' lesion detection and characterization ability using breast ultrasound. During the study, the team also assessed the impact of specific lesion features on diagnostic performance.
Investigators prepared six phantoms with 17 lesions measuring 2 to 10 mm, placed at different locations and depths. The phantoms were scanned and findings recorded by 66 radiologists at 23 institutions.
Of the 17 lesions, radiologists detected a median of 14 (82%). Larger lesions (5 to 10 mm) were most easily detected, by 97.5% of the radiologists. Detection declined respectively with size, with 83% of radiologists detecting 4-mm lesions, 71% identifying 3-mm lesions, and 44% correctly finding 2-mm lesions.
"Generally, ultrasound sensitivity was highest for lesions 5 to 10 mm," Berg said. "Lesions under 5 mm were less reliably detected and characterized."
Other features influencing detection included lesion depth. The deeper the lesion, the harder the identification, Berg said. Anechoic lesions also posed difficulties: Only 33% of the 3-mm lesions were so characterized.
During the three-year, $8 million ACRIN trial, investigators will study 2508 women at high risk for breast cancer using both mammography and ultrasound. In this initial phase, investigators focused only on interpretive performance factors.
"We expect that performance results using the phantom will be predictive of what we will see in clinical practice, but that will be confirmed once we are further along in the trial," Berg said.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.
















