
Practice mergers or acquisitions are quickly becoming more common, and a Diagnostic Imaging survey found most radiologists are concerned about the trend. Here's how best to handle it.

Practice mergers or acquisitions are quickly becoming more common, and a Diagnostic Imaging survey found most radiologists are concerned about the trend. Here's how best to handle it.
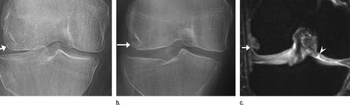
Researchers found the modality to be more proficient than radiography in identifying the hallmarks of knee osteoarthritis, but say it's still too early to recommend using tomosynthesis as a standard practice.
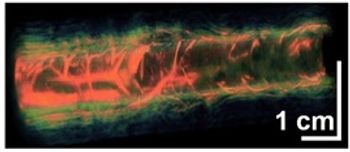
Researchers want to make photoacoustic tomography, which pairs light and sound, available to providers. Clinical trials are already under way to visualize sentinel lymph nodes for breast cancer staging – just one of several potential applications of this technology.

The biggest concern about viewing diagnostic studies on mobile devices has been screen resolution. The new iPad's “retina display” could change that.

Radiology groups bring increased worth through timely service, imaging expertise, high exam quality, expert interpretation, patient safety, and cost containment.

By eliminating the barriers that hamper clear communication and improving leadership skills from within, radiology departments can proactively improve how well they work with hospitals.

Changing reimbursement structures and different healthcare setting models have made understanding practice management and healthcare policy a must.

Jon Robins, MD, head of Imaging Healthcare Specialists in San Diego, discusses how his practice achieved far lower doses and and the impact the moves have had on the practice.

After being left out of the first phase of the meaningful use program, medical imaging was included in the proposed Stage 2 rule CMS and the Office of the National Coordinator released last week.
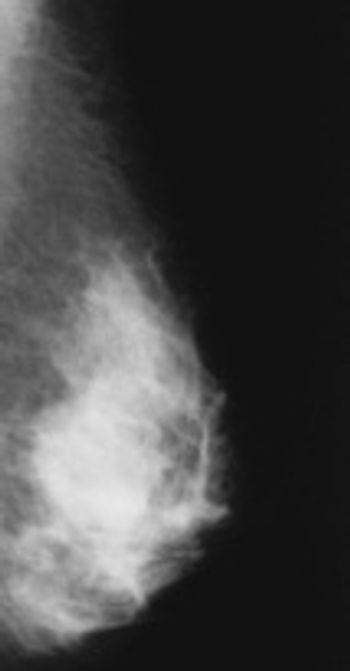
It’s been two years since Connecticut enacted a law requiring providers to tell patients in writing if they have dense breast tissue, and other states are following suit. But practitioners say complying with the law is often complicated.

As the details of healthcare reform begin to solidify, one this is clear: Radiologists must step up and assume greater leadership roles.

Some of the upcoming challenges touch the individual radiologist’s pocketbook; others affect practice. Regardless of the specifics, radiologists will do well to revamp how they view themselves as part of the healthcare system.
Starting July 1, diagnostic radiologists in California will be required to include radiation dose levels in all CT reports. Response has been mainly positive, but there are still concerns about the legislation's effect on daily practice.

California practices will be required to report CT dose starting July 1, and some are already seeing a culture change when it comes to radiation dose levels.

The rising popularity of sending images via the Internet doesn’t mean everyone in the radiology industry is comfortable with the idea. Yet experts say existing protocols are keeping images safe.

The number of mammography scans is rising, but the number of radiologists willing to read the studies is falling. Enter telemammography.

“It’s a beautiful thing. We can send images and set up connections on the fly as they’re needed,” said Gayle Knudson, Great Falls Clinic’s radiology manager.

Cloud-based image transfer eliminates the possibility that an image-containing CD will be lost when patients visit a new provider or clinical setting. Here's what you need to know about this growing trend.

Patient no-shows have long plagued the healthcare industry, and radiology is no exception. But there are tactics you can implement to reduce the no-show rate or recoup lost revenue.

Over the past 20 years, not only has clinical instruction during radiology residency changed, but so has the practice life that comes after it. Even as a growing number of medical students select radiology as a specialty, practice-setting preferences have shifted for your younger colleagues. They also have a different set of priorities to consider.

In the age of healthcare reform, boosting patient satisfaction with the services you provide is critical to reimbursement. Many of you have purchased open or wide-bore MRI machines with higher Tesla strength to make your claustrophobic patients more comfortable. Or maybe you’ve added a scanner just for children. But your imaging technology is only part of the fix, according to some in the industry.

A big buzzword in radiology currently is patient experience. Many practices have invested in updated machines and staff training to make sure the imaging process goes as smoothly for your patients as possible.

Mammography versus magnetic resonance imaging (MRI) has been a long-standing debate among industry leaders. The general consensus today, however, is while both tests effectively detect breast cancer and can work hand-in-hand, mammography is still indispensable.

Bringing your low-dose CT protocols down even further doesn’t have to mean tossing out your old scanners and buying pricey new ones. According to one San Diego-based imaging center, you can trim radiation doses to almost nothing and still get high-quality scans appropriate for diagnosis.

If you’ve seen fewer and fewer physicians referring patients to your center for imaging services over the past five years, you’re not alone. The decline is a nationwide trend, and many industry consultants believe that to fortify your bottom line, you must go on the offensive.

Many practices and hospital imaging departments nationwide are using manicures, wine, massages, and other activities to bring women in for their annual breast screenings. These so-called mammogram parties have received an extremely positive response from patients, officials said.

The Blue Cross Blue Shield Association plan unveiled last week that touches on advanced imaging services has industry leaders up-in-arms, calling for Congress to leave plan-of-care decisions between doctors and their patients.

MRI-related accidents and injury reporting are on the rise, prompting the FDA to examine thermal burns, projectiles, implantable devices, and hearing loss.

Social networking in healthcare isn’t new, but there is a growing trend to create groups focused on particular specialty areas. And radiology is in the middle of it all, with networks bringing together physicians and technologists alike.

Natural language processing, considered the next generation of voice recognition software, makes it easier for you to summarize, find, and retrieve data from radiology reports. But a recent study shows many of you still aren’t using it.