
The old adage about bad customer service experiences being shared with 10 other people may apply to objectionable hiring practices in radiology as well.

The old adage about bad customer service experiences being shared with 10 other people may apply to objectionable hiring practices in radiology as well.

While one may occasionally engage in tongue-in-cheek humor about righting wrongs in radiology, maintaining professional perspective remains the order of the day.

Autosave functionality for dictation software and availability of prior imaging are elusive yet very practical essentials that could eliminate a fair amount of redundancy with radiology reports.

Dwelling on a bad experience or episode with a referrer or colleague is never worth the sacrifice of perspective and forward momentum.

Proactive approaches to training, compensation issues and staff feedback are hallmarks for engaging and retaining top radiology staff.
Given a certain perception that calling out sick is frowned upon in health care, radiologists and other health care workers may feel conflicted about being absent even if an illness has reduced their capacity for getting work done on a given day.

A prospective employer’s willingness or unwillingness to negotiate notice periods in a contact may signal the difference between a worthwhile opportunity and a one-way, dead-end job.

Going beyond the humdrum, eye roll-inducing platitudes of orientation training may foster improved attention and adherence to training priorities such as cybersecurity.

Is it time to rethink the burden of applicant fees, credentialing costs and medical staff dues?

A singular database of current rules, guidelines and best practices in radiology would be a welcome advance to ensure ease of access, consistency, and proactive prevention of frivolous malpractice cases.

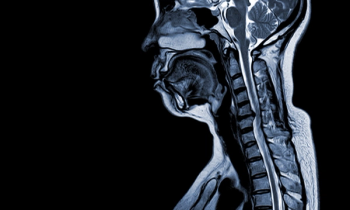
While CT, MRI and X-rays provide more of a workout for one’s radiological skills, more occasional spurts of DEXA scans and Doppler ultrasounds can provide comfortable diversions on worklists.

A comfortable environment for reading CTs, MRIs and X-rays may be conducive to less interruptions and longer intervals at radiology workstations.

The will to provide legitimate make goods to help address bad situations for radiologist employers can be a key difference between staff loyalty or mutiny.

Catch up on the most well-read Eric Postal, M.D.-penned blogs from 2023.

Expressing appreciation for the technological advances that have limited previous disruptions to radiology workflow, this author speculates about what could come next with AI, voice recognition and workstation enhancements.
Excess verbiage, at the behest of non-clinical interlopers, continues to pervade radiology reports.

Can a return to a per-click reimbursement model reignite one’s drive?

Is it time to reassess what constitutes a never event?

Is there a certain hypochondriasis that may lead some radiologists to pursue their own imaging, and would it change how aggressively they follow up incidentalomas on their own scans?

The success of compliance initiatives is often preceded by an easily understood rationale and simply stated benefits.

While some may see a job applicant with multiple past employers as a job hopper, others may see an opportunity to hire a radiologist with diverse work experience.

Is the continued rise of artificial intelligence (AI) driven by legitimate “machine learning,” or do the frequently “suspicious” chest X-rays and questionable detection of subtle findings on head CTs reveal a hype-driven train of new products with an ultimately “planned obsolescence”?

What constitutes an optimal work schedule in radiology?

While this author has no intention of retiring from radiology, he notes that retiring from certain work schedules or aspects of the field have had a favorable impact on his life.

While there may be awkwardness and a degree of embarrassment in noting obvious findings to referring clinicians in radiology, consistent communication of those findings is essential.

How strong is your own quality assurance (QA) barometer for interpreting CT, MRI, and ultrasound images?

I’ve long since learned that good faith is far more reliable than, say, contracts.

When facilities routinely forward X-rays for “pain,” vascular ultrasound studies without Doppler or chest computed tomography (CT) scans devoid of breath holding, patient care suffers.
When you are asked for an informal medical opinion, one’s intellectual curiosity and desire to help others never fade away.
What do you do with a CD of imaging that has no information on the doc requesting the radiologist read?