
Researchers found that Korean women with a combination of benign breast disease and BI-RADS category C or BI-RADS category D breast density had a nearly threefold or greater 10-year risk for breast cancer.

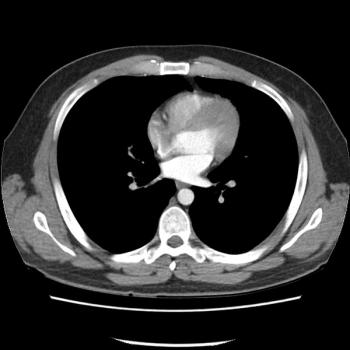
In a recent video interview on the current iodinated contrast media shortage, neuroradiologist Sean Bryant, MD discussed imaging alternatives, emphasized communication with referring physicians on optimal studies, and discussed the ongoing need to prevent “protocol creep” with timely updates of imaging protocols.

GE Healthcare to Resume 'Close to 100 Percent' Production of Iodinated Contrast Media Products This Week
Can Pre-COVID Medicare Claims Data Improve Mitigation Targets for the Iodinated Contrast Media Shortage?

Researchers found that Korean women with a combination of benign breast disease and BI-RADS category C or BI-RADS category D breast density had a nearly threefold or greater 10-year risk for breast cancer.
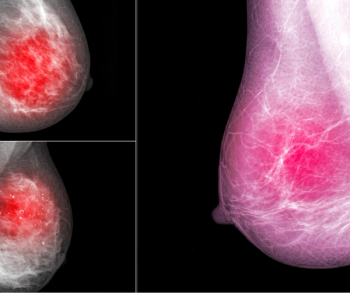
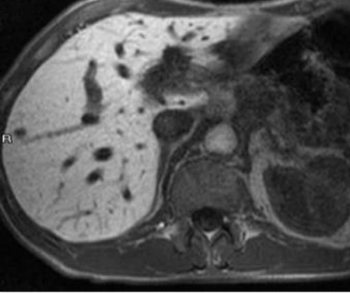
In a recent lecture at the Society of Breast Imaging (SBI)/American College of Radiology (ACR) conference, Linda Moy, MD, reviewed key tips for optimizing magnetic resonance imaging (MRI) of the breast.
Could the emerging artificial intelligence platforms Saige-Dx and Quantib Prostate 2.0 improve cancer detection with mammography and prostate MRI?

Is it a thoughtless verbal reflex or a failure to go beyond a surface read of imaging?

Catch up on the top radiology content of the past week.
Given the challenges with the shortage of the iodinated contrast agent Omnipaque, national and state organizations have issued suggested risk mitigation and conservation strategies to reprioritize imaging needs during this temporary shortage.

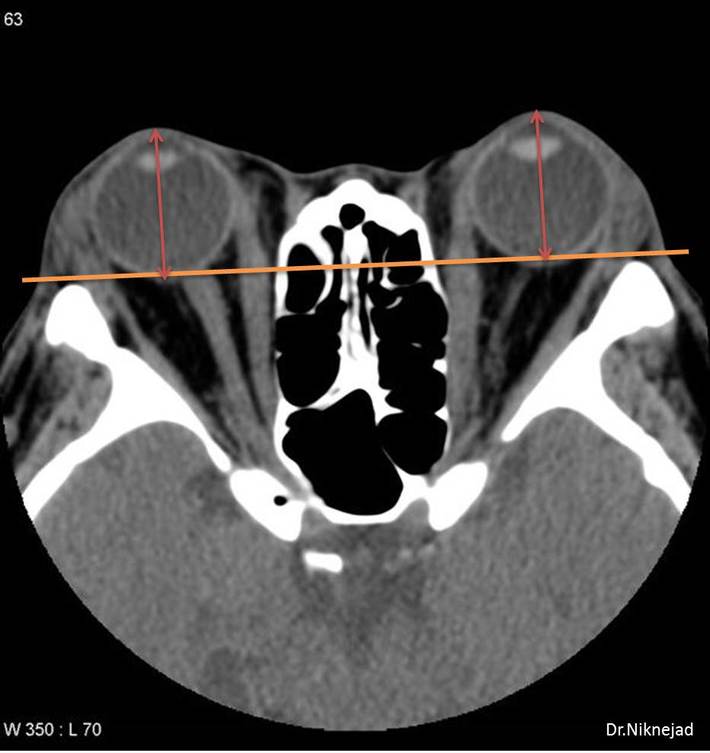
What is the diagnosis?
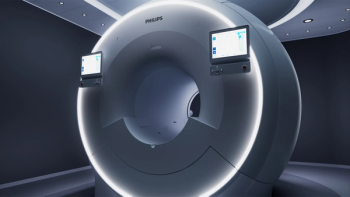
Offering integrated artificial intelligence (AI) and seamless multi-nuclei imaging capabilities, the new magnetic resonance imaging (MRI) system reportedly enhances image quality and workflow efficiency.

Review the top radiology content from the past week.

While there can be an array of challenges in outsourcing night coverage to teleradiology service providers, due diligence with contract terms can help mitigate costs and increase flexibility if radiology practices decide to switch teleradiology providers down the line.
Could an emerging modality provide a viable alternative to gadolinium-based contrast agents (GBCAs) in this high-risk patient population?

Review top radiology content from the week.
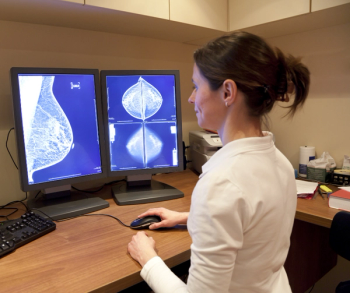
Validating a prognostic scoring system for locoregional recurrence risk in post-mastectomy patients with varying levels of axillary lymph node involvement, emerging research suggests patients with intermediate risk for breast cancer recurrence could benefit from post-mastectomy radiotherapy.

Review top radiology content from the week.
In a recent video interview, Arun Krishnaraj, MD, MPH and David Larson, MD, MBA, discussed the continued use of physical media to transport medical images between different health-care facilities, resulting inefficiencies and delays with patient care, and the initiative to create a linked multi-hub model to end this dated practice once and for all.
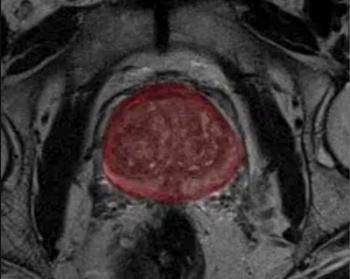
In addition to segmentation of the prostate, the artificial intelligence (AI)-enabled advance reportedly facilitates PI-RADS scoring by assessing the size and intensity of possible lesions.

Review top radiology content from the week.

Review top radiology content from the week.

The new whole-body magnetic resonance imaging (MRI) platform reportedly offers enhanced image quality and increased patient comfort.

Given the broad range of fibrocystic changes, the authors of a recent study suggest that more precise diagnosis of breast MRIs could significantly reduce unnecessary biopsy procedures.
Study findings further highlight the central role of PET/CT in disease response after CAR-T cell therapy.
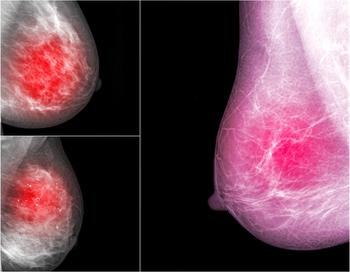
Diffusion-weighted imaging may be useful as a safe and effective screening tool to supplement mammography in women with dense breast tissues.
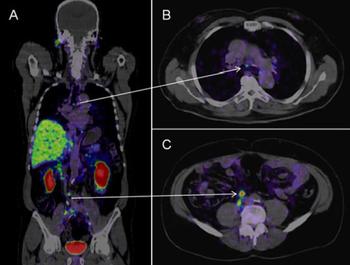
PSMA PET is highly robust in identifying prostate cancer lesions which are otherwise deemed unremarkable.

Multiparametric MRI can detect pathologic complete response after neoadjuvant therapy in patients with esophageal squamous cell carcinoma.

Breast ultrasound/MRI fusion significantly improves localization of incidentally detected MRI lesions which are occult on an initial ultrasound survey alone.